5 Vesicoureteral Reflux (VUR) Nursing Care Plans
Meconium Aspiration Syndrome
13 Surgery (Perioperative Client) Nursing Care Plans
Nursing Prioritization, Delegation and Assignment #6: Fluid, Electrolyte, and Acid-Base Imbalances (20 Questions)
NCLEX Practice Exam 1 (40 Questions)
NCLEX-RN Cram Sheet for Nursing Exams (2019 Update)
Ineffective Tissue Perfusion
Risk for Electrolyte Imbalance
10 Geriatric (Older Adult) Nursing Care Plans
Normal Laboratory Values Guide
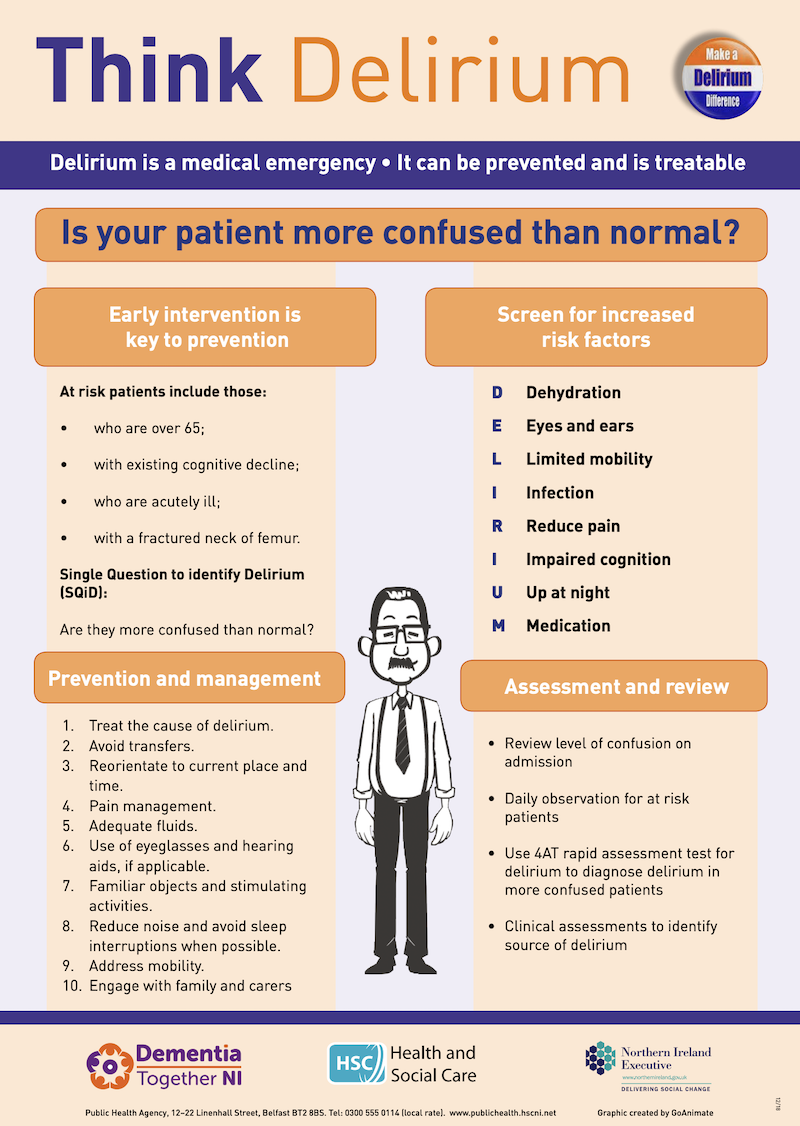
Delirium
My grandfather has turned 89 years old 2 months ago. He seems to have changed from then on. He always complains of seeing ants in the ceiling, or ants on the floor beside his bed. He sometimes forgets my name. Lately, he keeps on mumbling to himself and looks agitated. He doesn’t know where he is anymore, or what the present date is. I’m really worried that he is in the early stages of delirium. I think we should have him checked.
Description
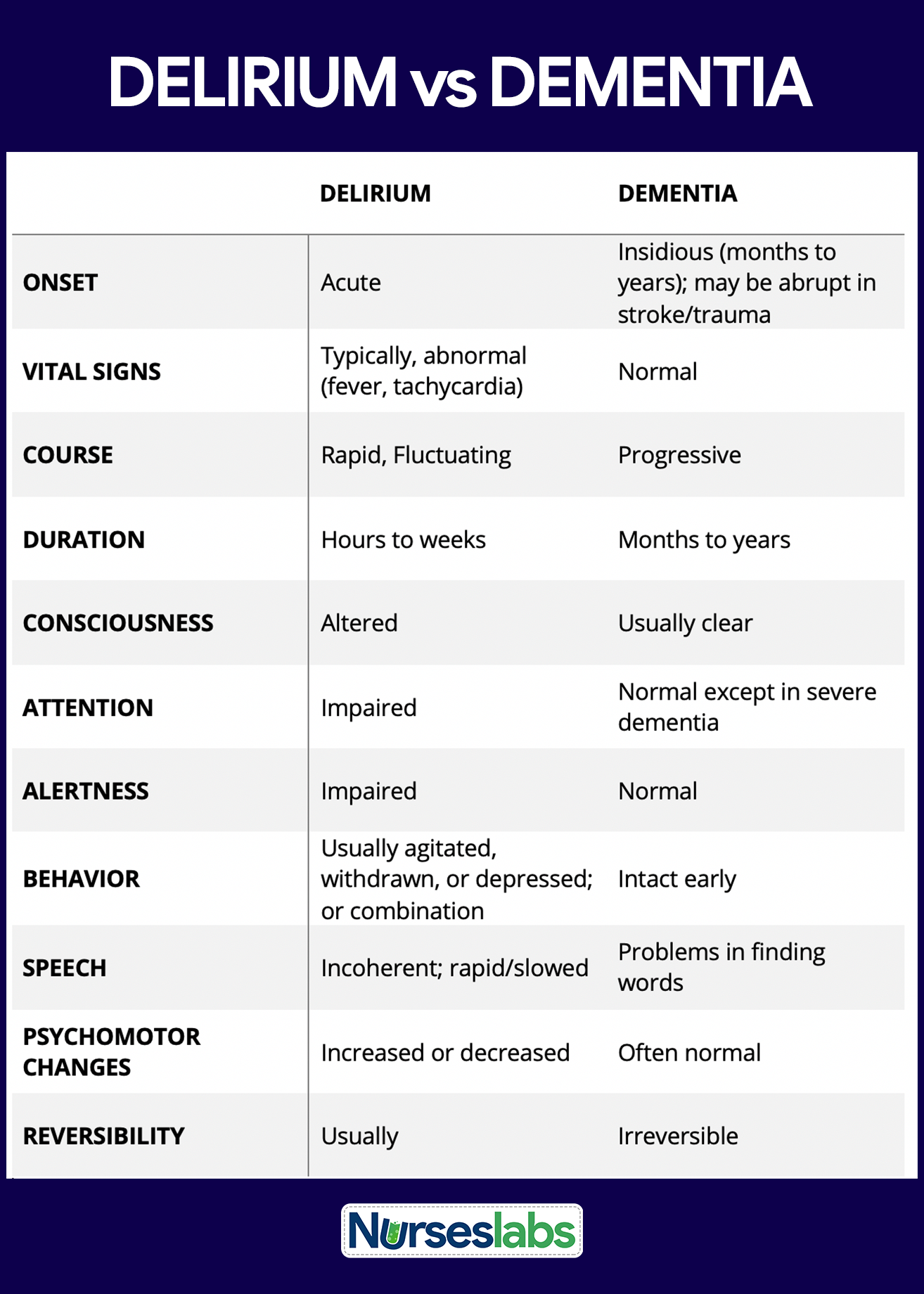
Delirium is a disturbance of consciousness and a change in cognition that develop rapidly over a short period (DSM-IV-TR).
Statistics and Incidences
Delirium is common in the United States.
- In a systematic review of 42 cohorts in 40 studies, 10-31% of new hospital admissions met the criteria for delirium and the incidence of developing delirium during the admission ranged from 3-29%.
- For patients in intensive care units, the prevalence of delirium may reach as high as 80%.
- Prevalence of postoperative delirium following general surgery is 5-10% and as high as 42% following orthopedic surgery.
- As many as 80% of patients develop delirium death.
- Delirium can occur at any age, but it occurs more commonly in patients who are elderly and have compromised mental status.
- In patients who are admitted with delirium, mortality rates are 10-26%.
- Patients who develop delirium during hospitalization have a mortality rate of 22-76% and a high rate of death during the months following discharge.
Causes
The DSM-IV-TR differentiates among the disorders of delirium by their etiology, although they share a common symptom presentation. Categories of delirium include the following:
- Delirium due to a general medical condition. Certain medical conditions, such as systemic infections, metabolic disorders, fluid and electrolyte imbalances, liver or kidney disease, thiamine deficiency, postoperative states, hypertensive encephalopathy, postictal states, and sequelae of head trauma, can cause symptoms of delirium.
- Substance-induced delirium. The symptoms of delirium can be induced by exposure to a toxin or the ingestion of medications, such as anticonvulsants, neuroleptics, anxiolytics, antidepressants, cardiovascular medications, antineoplastics, analgesics, antiasthmatic agents, antihistamines, antiparkinsonian drugs, corticosteroids, and gastrointestinal medications.
- Substance-intoxication delirium. Delirium symptoms can occur in response to taking high doses of cannabis, cocaine, hallucinogens, alcohol, anxiolytics, or narcotics.
- Substance-withdrawal delirium. Reduction or termination of long-term, high dose, use of certain substances, such as alcohol, sedatives, hypnotics, or anxiolytics, can result in withdrawal delirium symptoms.
- Delirium due to multiple etiologies. Symptoms of delirium may be related to more than one general medical condition or to the combined effects of a general medical condition and substance use.
Clinical Manifestations
The following symptoms have been identified with the syndrome of delirium:
- Altered consciousness ranging from hypervigilance to stupor or semicoma.
- Extreme distractibility with difficulty focusing attention.
- Disorientation to time and place.
- Impaired reasoning ability and goal-directed behavior.
- Disturbance in the sleep-wake cycle.
- Emotional instability as manifested by fear, anxiety, depression, irritability, anger, euphoria, or apathy.
- Misperceptions of the environment, including illusions and hallucinations.
- Automatic manifestations, such as tachycardia, sweating, flushed face, dilated pupils, and elevated blood pressure.
- Incoherent speech.
- Impairment of recent memory.
Assessment and Diagnostic Findings
Laboratory tests that may be helpful for diagnosis include the following:
- Complete blood cell count with differential. Helpful to diagnose infection and anemia.
- Electrolytes. To diagnose low or high levels.
- Glucose. To diagnose hypoglycemia, diabetic ketoacidosis, and hyperosmolar nonketotic states.
- Renal and liver function tests. To diagnose renal and liver failure.
- Thyroid function studies. To diagnose hypothyroidism.
- Urine analysis. Used to diagnose urinary tract infection.
- Urine and blood drug screen. Used to diagnose toxicological causes.
- Thiamine and vitamin B12 levels. Used to detect deficiency states of these vitamins.
- Serum marker for delirium. The calcium binding protein S-100 B could be a serum marker for delirium. Higher levels are seen in patients with delirium when compared to patients without delirium.
Medical Management
When delirium is diagnosed or suspected, the underlying causes should be sought and treated.
- Fluid and nutrition. Fluid and nutrition should be given carefully because the patient may be unwilling or physically unable to maintain a balanced intake; for the patient suspected of having alcohol toxicity or alcohol withdrawal, therapy should include multivitamins, especially thiamine.
- Reorientation techniques. Reorientation techniques or memory cues such as a calendar, clicks, and family photos may be helpful.
- Supportive therapy. The environment should be stable, quiet, and well-lighted; sensory deficits should be corrected, if necessary, with eyeglasses or hearing aids; family members and staff should explain proceedings at every opportunity, reinforce orientation, and reassure the patient.
Pharmacologic Management
Delirium that causes injury to the patient or others should be treated with medications.
- Antipsychotics. This class of drugs is the medication of choice in the treatment of psychotic symptoms of delirium.
- Benzodiazepines. Reserved for delirium resulting from seizures or withdrawal from alcohol or sedative hypnotics.
- Vitamins. Patients with alcoholism and patients with malnutrition are prone to thiamine and vitamin B12 deficiency, which can cause delirium.
- Hypnotic, miscellaneous. Agents in this class may be useful in the prevention and management of delirium (e.g. melatonin, ramelteon).
Nursing Management
Nursing management for a patient with delirium include the following:
Nursing Assessment
Nursing assessment should include:
- Psychiatric interview. The psychiatric interview must contain a description of the client’s mental status with a thorough description of behavior, flow of thought and speech, affect, thought processes and mental content, sensorium and intellectual resources, cognitive status, insight, and judgment.
- Serial assessment. Serial assessment of psychiatric status is necessary for determining fluctuating course and acute changes in mental status.
Nursing Diagnosis
NANDA nursing diagnoses for persons with delirium include:
- Disturbed thought processes related to delusional thinking.
- Chronic Confusion related to cognitive impairment.
- Impaired verbal communication related to cognitive impairment.
- Risk for injury related to suicidal ideations, illusions, hallucinations.
- Impaired memory related to cognitive impairment.
- Risk for other-directed violence related to suspiciousness of others.
Nursing Care Planning and Goals
The major nursing care plan goals for delirium are:
- Client will maintain agitation at a manageable level so as not to become violent.
- Client will not harm self or others.
Nursing Interventions
Nursing interventions for patients with delirium include the following:
- Assess level of anxiety. Assess client’s level of anxiety and behaviors that indicate the anxiety is increasing; recognizing these behaviors, nurse may be able to intervene before violence occurs.
- Provide an appropriate environment. Maintain a low level of stimuli in client’s environment (low lighting, few people, simple decor, low noise level) because anxiety increases in a highly stimulating environment.
- Promote patient’s safety. Remove all potentially dangerous objects from client’s environment; in a disoriented, confused state, clients may use objects to harm self or others.
- Ask assistance from others when needed. Have sufficient staff available to execute a physical confrontation, if necessary; assistance may be required from others to provide for physical safety of client or primary nurse or both.
- Stay calm and reassure patient. Maintain a calm manner with the client; attempt to prevent frightening client unnecessarily; Provide continual reassurance and support.
- Interrupt periods of unreality and reorient; client safety is jeopardized during periods of disorientation; correcting misinterpretations of reality enhances client’s feelings of self-worth and personal dignity.
- Medicate or restrain patient as prescribed. Use tranquilizing medications and soft restraints, as prescribed by physician, for protection of client and other during periods of elevated anxiety.
- Observe suicide precautions. Sit with client and provide one-to-one observation if assessed to be actively suicidal; client safety is a nursing priority, and one-to-one observation may be necessary to prevent a suicidal attempt.
- Teach relaxation exercises to intervene in times of increasing anxiety.
- Teach prospective caregivers to recognize client behaviors that indicate anxiety is increasing and ways to intervene before violence occurs.
Evaluation
The outcome criteria includes:
- Prospective caregivers are able to verbalize behaviors that indicate an increasing anxiety level and ways they may assist client to manage the anxiety before violence occurs.
- With assistance from caregivers, client is able to control impulse to perform acts of violence against self or others.
Documentation Guidelines
Documentation in a patient with delirium include:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Practice Quiz: Delirium
Nursing practice questions for delirium. For more practice questions, visit our NCLEX practice questions page.
Exam Mode
In Exam Mode: All questions are shown but the results, answers, and rationales (if any) will only be given after you’ve finished the quiz.
Practice Quiz: Delirium
Practice Mode
Practice Mode: This is an interactive version of the Text Mode. All questions are given in a single page and correct answers, rationales or explanations (if any) are immediately shown after you have selected an answer. No time limit for this exam.
Practice Quiz: Delirium
Text Mode
Text Mode: All questions and answers are given on a single page for reading and answering at your own pace. Be sure to grab a pen and paper to write down your answers.
1. Nurse Josefina is caring for a client who has been diagnosed with delirium. Which statement about delirium is true?
A. It’s characterized by an acute onset and lasts about 1 month.
B. It’s characterized by a slowly evolving onset and lasts about 1 week.
C. It’s characterized by a slowly evolving onset and lasts about 1 month.
D. It’s characterized by an acute onset and lasts hours to a number of days.
1. Answer: D. It’s characterized by an acute onset and lasts hours to a number of days
- D: Delirium has an acute onset and typically can last from several hours to several days.
2. Edward, a 66-year-old client with slight memory impairment and poor concentration, is diagnosed with primary degenerative dementia of the Alzheimer’s type. Early signs of this dementia include subtle personality changes and withdrawal from social interactions. To assess for progression to the middle stage of Alzheimer’s disease, the nurse should observe the client for:
A. Occasional irritable outbursts.
B. Impaired communication.
C. Lack of spontaneity.
D. Inability to perform self-care activities.
2. Answer: B. Impaired communication.
- B: Signs of advancement to the middle stage of Alzheimer’s disease include exacerbated cognitive impairment with obvious personality changes and impaired communication, such as inappropriate conversation, actions, and responses.
- A and C: Initially, memory impairment may be the only cognitive deficit in a client with Alzheimer’s disease. During the early stage of this disease, subtle personality changes may also be present. However, other than occasional irritable outbursts and lack of spontaneity, the client is usually cooperative and exhibits socially appropriate behavior.
- D: During the late stage, the client can’t perform self-care activities and may become mute.
3. Loretta, a newly admitted client was diagnosed with delirium and has a history of hypertension and anxiety. She had been taking digoxin, furosemide (Lasix), and diazepam (Valium) for anxiety. This client’s impairment may be related to which of the following conditions?
A. Infection
B. Metabolic acidosis
C. Drug intoxication
D. Hepatic encephalopathy
3. Answer: C. Drug intoxication.
- C: This client was taking several medications that have a propensity for producing delirium; digoxin (a digitalis glycoside), furosemide (a thiazide diuretic), and diazepam (a benzodiazepine).
- A, B, and D: Sufficient supporting data don’t exist to suspect the other options as causes.
4. Nurse Ron enters a client’s room, the client says, “They’re crawling on my sheets! Get them off my bed!” Which of the following assessment is the most accurate?
A. The client is experiencing aphasia.
B. The client is experiencing dysarthria.
C. The client is experiencing a flight of ideas.
D. The client is experiencing visual hallucination.
4. Answer: D. The client is experiencing visual hallucination.
- D: The presence of a sensory stimulus correlates with the definition of a hallucination, which is a false sensory perception.
- A: Aphasia refers to a communication problem.
- B: Dysarthria is difficulty in speech production.
- C: Flight of ideas is rapid shifting from one topic to another.
5. Which of the following descriptions of a client’s experience and behavior can be assessed as an illusion?
A. The client tries to hit the nurse when vital signs must be taken.
B. The client says, “I keep hearing a voice telling me to run away.”
C. The client becomes anxious whenever the nurse leaves the bedside.
D. The client looks at the shadow on a wall and tells the nurse she sees frightening faces on the wall.
5. Answer: D. The client looks at the shadow on a wall and tells the nurse she sees frightening faces on the wall.
- D: Minor memory problems are distinguished from dementia by their minor severity and their lack of significant interference with the client’s social or occupational lifestyle.
- A, B, and C: Other options would be included in the history data but don’t directly correlate with the client’s lifestyle.
References
Sources and references for this study guide for delirium:
- Black, J. M., & Hawks, J. H. (2005). Medical-surgical nursing. Elsevier Saunders,.
- Videbeck, S. L. (2010). Psychiatric-mental health nursing. Lippincott Williams & Wilkins.
Dementia
“Maud Shade was eighty when a sudden hush
Fell on her life. We saw the angry flush
And torsion of paralysis assail
Her noble cheek. We moved her to Pinedale,
Famed for its sanitarium. There she’d sit
In the glassed sun and watch the fly that lit
Upon her dress and then upon her wrist.
Her mind kept fading in the growing mist.
She still could speak. She paused, and groped, and found
What seemed at first a serviceable sound,
But from adjacent cells impostors took
The place of words she needed, and her look
Spelt imploration as she fought in vain
To reason with the monsters in her brain.”
― Vladimir Nabokov, Pale Fire
What is Dementia?
Dementia is defined by a loss of previous levels of cognitive, executive, and memory function in a state of full alertness (Bourgeois, Seaman, & Servis, 2008).
- Dementia has a slow, insidious onset, and is chronic, progressive, and irreversible.
Statistics and Incidences
Cases of dementia are increasing due to longer life expectancy of the world population.
- There are four clinical dementia syndromes accounting for 90% of all cases after excluding other common reversible causes of cognitive impairment.
- The rise in dementia and Alzheimer’s disease is alarming and is expected to double every 20 years, from 47 million people in 2015 to 75 million people in 2030 and 131 million in 2050.
Causes
Following are major etiologic categories for the syndrome of dementia:
- Dementia of the Alzheimer’s type. The exact disease of Alzheimer’s disease is unknown, but several theories have been proposed, such as reduction in brain acetylcholine, the formation of plaques and tangles, serious head trauma, and genetic factors. Pathologic changes in the brain include atrophy, enlarged ventricles, and the presence of numerous neurofibrillary plaques and tangles.
- Vascular Dementia. This type of dementia is caused by significant cerebrovascular disease. The client suffers the equivalent of small strokes caused by arterial hypertension or cerebral emboli or thrombi, which destroy many areas of the brain. The onset of symptoms is more abrupt than in AD and runs a highly variable course, progressing in steps rather than a gradual deterioration.
- Dementia due to HIV disease. The immune dysfunction associated with human immunodeficiency virus (HIV) can lead to brain infections by other organisms. HIV also appears to cause dementia directly.
- Dementia due to head trauma. The syndrome of symptoms associated with dementia can be brought on by a traumatic head injury.
- Dementia due to Lewy Body Disease. Clinically, Lewy Body disease is fairly similar to AD,; however, it tends to progress more rapidly, and there is an earlier appearance of visual hallucinations and parkinsonian features (Rabins et al, 2006). This disorder is distinctive by the presence of Lewy bodies-eosinophilic inclusion bodies- seen in the cerebral cortex and brainstem (Andreasen and Black, 2006).
- Dementia due to Parkinson’s disease. Parkinsons’s disease is caused by a loss of nerve cells in the substantia nigra of the basal ganglia. The symptoms of dementia associated with Parkinson’s disease closely resemble those of AD.
- Dementia due to Huntington’s disease. This disease is transmitted as a Mendelian dominant gene, and damage occurs in the areas of the basal ganglia and the cerebral cortex.
- Dementia due to Pick’s disease. Pathology occurs from atrophy in the frontal and temporal lobes of the brain. Symptoms are strikingly similar to those of AD, and Pick’s disease is often misdiagnosed as AD.
- Dementia due to Creutzfeldt-Jakob disease. This form of dementia is caused by a transmissible agent known as a “slow virus” or prion. The clinical presentation is typical of the syndrome of dementia and the course is extremely rapid, with progressive deterioration and death within one year after onset.
- Dementia due to other general medical conditions. A number of other general medical conditions can cause dementia. Some of these include endocrine conditions, pulmonary disease, hepatic or renal failure, cardiopulmonary insufficiency, fluid and electrolyte imbalances, nutritional deficiencies, frontal or temporal lobe lesions, uncontrolled epilepsy, central nervous system or systemic infections, and other neurological conditions.
- Substance-induced Persisting Dementia. This type of dementia is related to the persisting effects of substances such as alcohol, inhalants, sedatives, hypnotics, anxiolytics, other medications, and environmental toxins.
Clinical Manifestations
The following symptoms have been identified with the syndrome of dementia:
- Memory impairment. Impaired ability to learn new information or to recall previously learned information.
- Impairment in abstract thinking, judgment, and impulse control.
- Impairment in language ability, such as difficulty naming objects. In some instances, the individual may not speak at all (aphasia).
- Personality changes are common.
- Impaired ability to perform motor activities despite intact motor abilities (apraxia).
- Disorientation. Patient may feel disoriented regarding current place, time, o names of persons they are close with.
- Wandering. Because of disorientation, patient with dementia may often wander from one place to another.
- Delusions are common (particularly delusions of persecution).
Assessment and Diagnostic Findings
Laboratory tests can be performed to rule out other conditions that may cause cognitive impairment.
- Complete blood cell count (CBC). Abnormalities in complete blood cell count and cobalamin levels require further workup to rule out hematologic disease.
- Liver enzyme levels. Abnormalities found in screening of liver enzyme levels require further workup to rule out hepatic disease.
- Thyroid-stimulating hormone (TSH) levels. Abnormalities in thyroid-stimulating hormone levels require further workup to rule thyroid disease.
- Rapid plasma reagent. Abnormalities in rapid plasma reagent (RPR) require further workup to rule out syphilis.
- HIV serology. Abnormalities in HIV serology and/or PCR require further workup to rule out HIV/AIDS.
- Paraneoplastic antibodies. Abnormalities in paraneoplastic antibodies require further workup to rule out autoimmune encephalitis.
- CSF proteins. Abnormalities in CSF proteins tau, P-tau, and 14-3-3 require further workup to rule out Creutzfeldt-Jakob disease.
Medical Management
To date, only symptomatic therapies are available and thus do not act on the evolution of the disease.
- Experimental therapies. A variety of experimental therapies have been proposed for dementia; these include anti-amyloid therapy, reversal of excess tau phosphorylation, estrogen therapy, vitamin E therapy, and free radical scavenger therapy; however, results of these studies have yielded disappointing results.
- Dietary measures. There are no special dietary considerations for dementia; however, caprylidene (Axona) is a prescription medical food that is metabolized into ketone bodies, and the brain can use these ketone bodies for energy when its ability to process glucose is impaired. Brain-imaging scans of older adults and persons with dementia reveal dramatically decreased uptake of glucose.
- Physical activity. Routine physical activity and exercise may have an impact on dementia progression and may perhaps have a protective effect on brain health; the patient’s surroundings should be safe and familiar; maintaining structured routines may be helpful to decrease patient’s stress in regard to meals, medication, and other therapeutic activities aimed at maintaining cognitive functioning.
Pharmacological Management
The mainstay of therapy for patients with dementia is the use of centrally acting cholinesterase inhibitors to attempt to compensate for the depletion of acetylcholine in the cerebral cortex and hippocampus.
- Cholinesterase inhibitors. Cholinesterase inhibitors are used to palliate cholinergic deficiency.
- N-Methyl-D-Aspartate antagonists. The only drug in the N-methyl-D-aspartate (NMDA) antagonist class that is approved by the US Food and Drug Administration is memantine; this agent may be used alone or in combination with AChE inhibitors.
- Nutritional supplement. Medical foods are dietary supplements intended to compensate specific nutritional problems caused by a disease or condition; caprylidene is indicated for clinical dietary management of metabolic processes associated with mild to moderate dementia.
Nursing Management
The nursing management of a client with dementia include the following:
Nursing Assessment
Assessment of a client with dementia include the following:
- Psychiatric interview. The psychiatric interview must contain a description of the client’s mental status with a thorough description of behavior, flow of thought and speech, affect, thought processes and mental content, sensorium and intellectual resources, cognitive status, insight, and judgment.
- Serial assessment. Serial assessment of psychiatric status is necessary for determining fluctuating course and acute changes in mental status, interviews with family members should be included and can be crucial in the treatment of infants and young children with cognitive disorders.
Nursing Diagnosis
Nursing diagnoses that you can use for developing nursing care plans for patients with dementia include:
- Risk for trauma related to disorientation or confusion.
- Risk for self-directed or other-directed violence related to delusional thinking.
- Chronic confusion related to alteration in structure/function of brain tissue.
- Self-care deficit related to cognitive impairment.
- Risk for falls related to cognitive impairment.
Nursing Care Planning and Goals
The major nursing care planning goals for dementia are:
- Client will accept explanations of inaccurate interpretation within the environment.
- With assistance from caregiver, client will be able to interrupt non-reality-based thinking.
Nursing Interventions
The nursing interventions for a dementia client are:
- Orient client. Frequently orient client to reality and surroundings. Allow client to have familiar objects around him or her; use other items, such as a clock, a calendar, and daily schedules, to assist in maintaining reality orientation.
- Encourage caregivers about patient reorientation. Teach prospective caregivers how to orient client to time, person, place, and circumstances, as required. These caregivers will be responsible for client safety after discharge from the hospital.
- Enforce with positive feedback. Give positive feedback when thinking and behavior are appropriate, or when client verbalizes that certain ideas expressed are not based in reality. Positive feedback increases self-esteem and enhances desire to repeat appropriate behavior.
- Explain simply. Use simple explanations and face-to-face interaction when communicating with client. Do not shout message into client’s ear. Speaking slowly and in a face-to-face position is most effective when communicating with an elderly individual experiencing a hearing loss.
- Discourage suspiciousness of others. Express reasonable doubt if client relays suspicious beliefs in response to delusional thinking. Discuss with the client the potential personal negative effects of continued suspiciousness of others.
- Avoid cultivation of false ideas. Do not permit rumination of false ideas. When this begins, talk to client about real people and real events.
- Observe client closely. Close observation of client’s behavior is indicated if delusional thinking reveals an intention for violence. Client safety is a nursing priority.
Evaluation
The outcome criteria for a patient with dementia include:
- With assistance from caregiver, client is able to distinguish between reality-based and non-reality based thinking.
- Prospective caregivers are able to verbalize ways in which to orient client to reality, as needed.
Documentation Guidelines
Documentation needed for a client with dementia include the following:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Practice Quiz: Dementia
Quiz time about the topic! For more practice questions, visit our NCLEX practice questions page.
Exam Mode
In Exam Mode: All questions are shown but the results, answers, and rationales (if any) will only be given after you’ve finished the quiz.
Practice Quiz: Dementia
Practice Mode
Practice Mode: This is an interactive version of the Text Mode. All questions are given in a single page and correct answers, rationales or explanations (if any) are immediately shown after you have selected an answer. No time limit for this exam.
Practice Quiz: Dementia
Text Mode
Text Mode: All questions and answers are given on a single page for reading and answering at your own pace. Be sure to grab a pen and paper to write down your answers.
1. Edward, a 66-year-old client with slight memory impairment and poor concentration, is diagnosed with primary degenerative dementia of the Alzheimer’s type. Early signs of this dementia include subtle personality changes and withdrawal from social interactions. To assess for progression to the middle stage of Alzheimer’s disease, the nurse should observe the client for:
A. Occasional irritable outbursts.
B. Impaired communication.
C. Lack of spontaneity.
D. Inability to perform self-care activities.
1. Answer: B. Impaired communication.
- Option B: Signs of advancement to the middle stage of Alzheimer’s disease include exacerbated cognitive impairment with obvious personality changes and impaired communication, such as inappropriate conversation, actions, and responses.
- Options A and C: Initially, memory impairment may be the only cognitive deficit in a client with Alzheimer’s disease. During the early stage of this disease, subtle personality changes may also be present. However, other than occasional irritable outbursts and lack of spontaneity, the client is usually cooperative and exhibits socially appropriate behavior.
- Option D: During the late stage, the client can’t perform self-care activities and may become mute.
2. Nurse Pauline is aware that Dementia, unlike delirium, is characterized by:
A. Slurred speech.
B. Insidious onset.
C. Clouding of consciousness.
D. Sensory perceptual change.
2. Answer: B. insidious onset.
- Option B: Dementia has a gradual onset and progressive deterioration. It causes pronounced memory and cognitive disturbances.
- Options A, C, and D: These are all characteristics of delirium.
3. The nurse is aware that the following ways in vascular dementia different from Alzheimer’s disease is:
A. Vascular dementia has more abrupt onset.
B. The duration of vascular dementia is usually brief.
C. Personality change is common in vascular dementia.
D. The inability to perform motor activities occurs in vascular dementia.
3. Answer: A. Vascular dementia has more abrupt onset.
- Option A: Vascular dementia differs from Alzheimer’s disease in that it has a more abrupt onset and runs a highly variable course.
- Option B: The duration of delirium is usually brief.
- Option C: Personality change is common in Alzheimer’s disease.
- Option D: The inability to carry out motor activities is common in Alzheimer’s disease.
4. A 65 years old client is in the first stage of Alzheimer’s disease. Nurse Patricia should plan to focus this client’s care on:
A. Offering nourishing finger foods to help maintain the client’s nutritional status.
B. Providing emotional support and individual counseling.
C. Monitoring the client to prevent minor illnesses from turning into major problems.
D. Suggesting new activities for the client and family to do together.
4. Answer: B. Providing emotional support and individual counseling.
- Option B: Clients in the first stage of Alzheimer’s disease are aware that something is happening to them and may become overwhelmed and frightened. Therefore, nursing care typically focuses on providing emotional support and individual counseling.
- Options A, C, and D: The other options are appropriate during the second stage of Alzheimer’s disease when the client needs continuous monitoring to prevent minor illnesses from progressing into major problems and when maintaining adequate nutrition may become a challenge. During this stage, offering nourishing finger foods helps clients to feed themselves and maintain adequate nutrition.
5. Nurse Kate would expect that a client with vascular dementia would experience:
A. Loss of remote memory related to anoxia.
B. Loss of abstract thinking related to emotional state.
C. Inability to concentrate related to decreased stimuli.
D. Disturbance in recalling recent events related to cerebral hypoxia.
5. Answer: D. Disturbance in recalling recent events related to cerebral hypoxia.
- Option D: Cell damage seems to interfere with registering input stimuli, which affects the ability to register and recall recent events; vascular dementia is related to multiple vascular lesions of the cerebral cortex and subcortical structure.
References
Sources and references for this study guide for delirium:
- Black, J. M., & Hawks, J. H. (2005). Medical-surgical nursing. Elsevier Saunders,.
- Videbeck, S. L. (2010). Psychiatric-mental health nursing. Lippincott Williams & Wilkins.
18 Heart Failure Nursing Care Plans
This nursing care plan guide contains 18 NANDA nursing diagnosis and some priority aspects of clinical care for patients with heart failure. Learn about the nursing interventions and assessment cues for heart failure including the goals, defining characteristics, and related factors for each nursing diagnosis.
What is Heart Failure?
Heart failure (HF) or Congestive Heart Failure (CHF) is a physiologic state in which the heart cannot pump enough blood to meet the metabolic needs of the body following any structural or functional impairment of ventricular filling or ejection of blood.
Heart failure results from changes in the systolic or diastolic function of the left ventricle. The heart fails when, because of intrinsic disease or structural it cannot handle a normal blood volume or, in absence of disease, cannot tolerate a sudden expansion in blood volume. Heart failure is a progressive and chronic condition that is managed by significant lifestyle changes and adjunct medical therapy to improve quality of life. Heart failure is caused by a variety of cardiovascular conditions such as chronic hypertension, coronary artery disease, and valvular disease.
Heart failure is not a disease itself, instead, the term refers to a clinical syndrome characterized by manifestations of volume overload, inadequate tissue perfusion, and poor exercise tolerance. Whatever the cause, pump failure results in hypoperfusion of tissues, followed by pulmonary and systemic venous congestion.
Clinical Manifestations
Heart failure can affect the heart’s left side, right side, or both sides. Though, it usually affects the left side first. The signs and symptoms of heart failure are defined based on which ventricle is affected—left-sided heart failure causes a different set of manifestations than right-sided heart failure.
Left-Sided Heart Failure
- Dyspnea on exertion
- Pulmonary congestion, pulmonary crackles
- Cough that is initially dry and nonproductive
- Frothy sputum that is sometimes blood-tinged
- Inadequate tissue perfusion
- Weak, thready pulse
- Tachycardia
- Oliguria, nocturia
- Fatigue
Right-Sided Heart Failure
- Congestion of the viscera and peripheral tissues
- Edema of the lower extremities
- Enlargement of the liver (hepatomegaly)
- Ascites
- Anorexia, nausea
- Weakness
- Weight gain (fluid retention)
Because heart failure causes vascular congestion, it is often called congestive heart failure, although most cardiac specialist no longer uses this term. Other terms used to denote heart failure include chronic heart failure, cardiac decompensation, cardiac insufficiency, and ventricular failure.
Nursing Care Plans
Nursing care plan goals for patients with heart failure includes support to improve heart pump function by various nursing interventions, prevention, and identification of complications, and providing a teaching plan for lifestyle modifications. Nursing interventions include promoting activity and reducing fatigue to relieve the symptoms of fluid overload.
Here are 18 nursing care plans (NCP) and nursing diagnosis for patients with Heart Failure:
- Decreased Cardiac Output
- Activity Intolerance
- Excess Fluid Volume
- Risk for Impaired Gas Exchange
- Risk for Impaired Skin Integrity
- Deficient Knowledge
- Acute Pain
- Ineffective Tissue Perfusion
- Hyperthermia
- Ineffective Breathing Pattern
- Ineffective Airway Clearance
- Impaired Gas Exchange
- Fatigue
- Risk for Decreased Cardiac Output
- Fear
- Anxiety
- Powerlessness
- Other Nursing Care Plans
Decreased Cardiac Output
The heart fails to pump enough blood to meet the metabolic needs of the body. The blood flow that supplies the heart is also decreased therefore decrease in cardiac output occurs, blood then is insufficient and making it difficult to circulate the blood to all parts of the body thus may cause altered heart rate and rhythm, weakness, and paleness.
Nursing Diagnosis
- Decreased Cardiac Output
Related Factors
- Altered myocardial contractility/inotropic changes
- Alterations in rate, rhythm, electrical conduction
- Structural changes (e.g., valvular defects, ventricular aneurysm)
- Poor cardiac reserve
- Side effects of medication
- Generalized weakness.
Defining Characteristics
- Increased heart rate (tachycardia), dysrhythmias, ECG changes
- Changes in BP (hypotension/hypertension)
- Extra heart sounds (S3, S4)
- Decreased urine output
- Diminished peripheral pulses
- Cool, ashen skin; diaphoresis
- Orthopnea, crackles, JVD, liver engorgement, edema
- Chest pain
Desired Outcomes
- Patient will demonstrate adequate cardiac output as evidenced by vital signs within acceptable limits, dysrhythmias absent/controlled, and no symptoms of failure (e.g., hemodynamic parameters within acceptable limits, urinary output adequate).
- Patient will report decreased episodes of dyspnea, angina.
- Patient will participate in activities that reduce cardiac workload.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Auscultate apical pulse, assess heart rate, rhythm. Document dysrhythmia if telemetry is available. | Tachycardia is usually present (even at rest) to compensate for decreased ventricular contractility. Premature atrial contractions (PACs), paroxysmal atrial tachycardia (PAT), PVCs, multifocal atrial tachycardia (MAT), and atrial fibrillation (AF) are common dysrhythmias associated with HF, although others may also occur.
Note: Intractable ventricular dysrhythmias unresponsive to medication suggest ventricular aneurysm. |
| Note heart sounds. | S1 and S2 may be weak because of diminished pumping action. Gallop rhythms are common (S3and S4), produced as blood flows into noncompliant chambers. Murmurs may reflect valvular incompetence. |
| Palpate peripheral pulses. | Decreased cardiac output may be reflected in diminished radial, popliteal, dorsalis pedis, and post tibial pulses. Pulses may be fleeting or irregular to palpation, and pulsus alternans (strong beat alternating with weak beat) may be present. |
| Monitor BP. | In early, moderate, or chronic HF, BP may be elevated because of increased SVR. In advanced HF, the body may no longer be able to compensate, and profound hypotension may occur. |
| Inspect skin for pallor, cyanosis. | Pallor is indicative of diminished peripheral perfusion secondary to inadequate cardiac output, vasoconstriction, and anemia. Cyanosis may develop in refractory HF. Dependent areas are often blue or mottled as venous congestion increases. |
| Monitor urine output, noting decreasing output and concentrated urine. | Kidneys respond to reduced cardiac output by retaining water and sodium. Urine output is usually decreased during the day because of fluid shifts into tissues but may be increased at night because fluid returns to circulation when patient is recumbent. |
| Note changes in sensorium: lethargy, confusion, disorientation, anxiety, and depression. | May indicate inadequate cerebral perfusion secondary to decreased cardiac output. |
| Assess for abnormal heart and lung sounds. | Allows detection of left-sided heart failure that may occur with chronic renal failure patients due to fluid volume excess as the diseased kidneys are unable to excrete water. |
| Monitor blood pressure and pulse. | Patients with renal failure are most often hypertensive, which is attributable to excess fluid and the initiation of the renin-angiotensin mechanism. |
| Assess mental status and level of consciousness. | The accumulation of waste products in the bloodstream impairs oxygen transport and intake by cerebral tissues, which may manifest itself as confusion, lethargy, and altered consciousness. |
| Assess patient’s skin temperature and peripheral pulses. | Decreased perfusion and oxygenation of tissues secondary to anemia and pump ineffectiveness may lead to decreased in temperature and peripheral pulses that are diminished and difficult to palpate. |
| Monitor results of laboratory and diagnostic tests. | Results of the test provide clues to the status of the disease and response to treatments. |
| Monitor oxygen saturation and ABGs. | Provides information regarding the heart’s ability to perfuse distal tissues with oxygenated blood |
| Therapeutic Interventions | |
| Give oxygen as indicated by patient symptoms, oxygen saturation and ABGs. | Makes more oxygen available for gas exchange, assisting to alleviate signs of hypoxia and subsequent activity intolerance. |
| Implement strategies to treat fluid and electrolyte imbalances. | Decreases the risk for development of cardiac output due to imbalances. |
| Administer cardiac glycoside agents, as ordered, for signs of left sided failure, and monitor for toxicity. | Digitalis has a positive isotropic effect on the myocardium that strengthens contractility, thus improving cardiac output. |
| Encourage periods of rest and assist with all activities. | Reduces cardiac workload and minimizes myocardial oxygen consumption. |
| Assist the patient in assuming a high Fowler’s position. | Allows for better chest expansion, thereby improving pulmonary capacity. |
| Teach patient the pathophysiology of disease, medications | Provides the patient with needed information for management of disease and for compliance. |
| Reposition patient every 2 hours | To prevent occurrence of bed sores |
| Instruct patient to get adequate bed rest and sleep | To promote relaxation to the body |
| Instruct the SO not to leave the client unattended | To ensure safety and reduce risk for falls that may lead to injury |
| Encourage rest, semirecumbent in bed or chair. Assist with physical care as indicated. | Physical rest should be maintained during acute or refractory HF to improve efficiency of cardiac contraction and to decrease myocardial oxygen demand/ consumption and workload. |
| Provide quiet environment: explain therapeutic management, help patient avoid stressful situations, listen and respond to expressions of feelings. | Psychological rest helps reduce emotional stress, which can produce vasoconstriction, elevating BP and increasing heart rate. |
| Provide bedside commode. Have patient avoid activities eliciting a vasovagal response (straining during defecation, holding breath during position changes). | Commode use decreases work of getting to bathroom or struggling to use bedpan. Vasovagal maneuver causes vagal stimulation followed by rebound tachycardia, which further compromises cardiac function. |
| Elevate legs, avoiding pressure under knee. Encourage active and passive exercises. Increase activity as tolerated. | Decreases venous stasis, and may reduce incidence of thrombus or embolus formation. |
| Check for calf tenderness, diminished pedal pulses, swelling, local redness, or pallor of extremity. | Reduced cardiac output, venous pooling, and enforced bed rest increases risk of thrombophlebitis. |
| Withhold digitalis preparation as indicated, and notify physician if marked changes occur in cardiac rate or rhythm or signs of digitalis toxicity occur. | Incidence of toxicity is high (20%) because of narrow margin between therapeutic and toxic ranges. Digoxin may have to be discontinued in the presence of toxic drug levels, a slow heart rate, or low potassium level. |
| Administer supplemental oxygen as indicated. | Increases available oxygen for myocardial uptake to combat effects of hypoxia. |
| Administer medications as indicated: | |
|
Diuretics, in conjunction with restriction of dietary sodium and fluids, often lead to clinical improvement in patients with stages I and II HF. In general, type and dosage of diuretic depend on cause and degree of HF and state of renal function. Preload reduction is most useful in treating patients with a relatively normal cardiac output accompanied by congestive symptoms. Loop diuretics block chloride reabsorption, thus interfering with the reabsorption of sodium and water. |
|
Vasodilators are the mainstay of treatment in HF and are used to increase cardiac output, reducing circulating volume (venodilators) and decreasing SVR, thereby reducing ventricular workload. Note: Parenteral vasodilators (Nitroprusside) are reserved for patients with severe HF or those unable to take oral medications. |
|
ACE inhibitors represent first-line therapy to control heart failure by decreasing ventricular filling pressures and SVR while increasing cardiac output with little or no change in BP and heart rate. |
|
Antihypertensive and cardioprotective effects are attributable to selective blockade of AT1(angiotensin II) receptors and angiotensin II synthesis. |
|
Increases force of myocardial contraction when diminished contractility is the cause of HF, and slows heart rate by decreasing conduction velocity and prolonging refractory period of the atrioventricular (AV) junction to increase cardiac efficiency /output. |
|
These medications are useful for short-term treatment of HF unresponsive to cardiac glycosides, vasodilators, and diuretics in order to increase myocardial contractility and produce vasodilation. Positive inotropic properties have reduced mortality rates 50% and improved quality of life. |
|
Useful in the treatment of HF by blocking the cardiac effects of chronic adrenergic stimulation. Many patients experience improved activity tolerance and ejection fraction. |
|
Decreases vascular resistance and venous return, reducing myocardial workload, especially when pulmonary congestion is present. Allays anxiety and breaks the feedback cycle of anxiety to catecholamine release to anxiety. |
|
Promote rest, reducing oxygen demand and myocardial workload. |
|
May be used prophylactically to prevent thrombus and embolus formation in presence of risk factors such as venous stasis, enforced bed rest, cardiac dysrhythmias, and history of previous thrombotic episodes. |
| Administer IV solutions, restricting total amount as indicated. Avoid saline solutions. | Because of existing elevated left ventricular pressure, patient may not tolerate increased fluid volume (preload). Patients with HF also excrete less sodium, which causes fluid retention and increases myocardial workload. |
| Monitor and replace electrolytes. | Fluid shifts and use of diuretics can alter electrolytes (especially potassium and chloride), which affect cardiac rhythm and contractility. |
| Monitor serial ECG and chest x-ray changes. | ST segment depression and T wave flattening can develop because of increased myocardial oxygen demand, even if no coronary artery disease is present. Chest x-ray may show enlarged heart and changes of pulmonary congestion. |
| Measure cardiac output and other functional parameters as indicated. | Cardiac index, preload, afterload, contractility, and cardiac work can be measured noninvasively by using thoracic electrical bioimpedance (TEB) technique. Useful in determining effectiveness of therapeutic interventions and response to activity. |
| Monitor laboratory studies: | |
|
Elevation of BUN or creatinine reflects kidney hypoperfusion. |
|
May be elevated because of liver congestion and indicate need for smaller dosages of medications that are detoxified by the liver. |
|
Measures changes in coagulation processes or effectiveness of anticoagulant therapy. |
|
May be necessary to correct bradydysrhythmias unresponsive to drug intervention, which can aggravate congestive failure and/or produce pulmonary edema. |
| Prepare for surgery as indicated: | |
|
Heart failure due to ventricular aneurysm or valvular dysfunction may require aneurysmectomy or valve replacement to improve myocardial contractility/ function. Revascularization of cardiac muscle by CABG may be done to improve cardiac function. |
|
Cardiomyoplasty, an experimental procedure in which the latissimus dorsi muscle is wrapped around the heart and electrically stimulated to contract with each heartbeat, may be done to augment ventricular function while the patient is awaiting cardiac transplantation or when transplantation is not an option. |
|
Other new surgical techniques include transmyocardial revascularization (percutaneous [PTMR]) using CO2 laser technology, in which a laser is used to create multiple 1-mm diameter channels in viable but underperfused cardiac muscle. |
| Assist with mechanical circulatory support system, such as IABP or VAD, when indicated. | An intra-aortic balloon pump (IABP) may be inserted as a temporary support to the failing heart in the critically ill patient with potentially reversible HF. A battery-powered ventricular assist device (VAD) may also be used, positioned between the cardiac apex and the descending thoracic or abdominal aorta. This device receives blood from the left ventricle (LV) and ejects it into the systemic circulation, often allowing patient to resume a nearly normal lifestyle while awaiting heart transplantation. With end-stage HF, cardiac transplantation may be indicated. |
Activity Intolerance
As heart failure becomes more severe, the heart is unable to pump the amount of blood required to meet all of the body’s needs. To compensate, blood is diverted away from less-crucial areas, including the arms and legs, to supply the heart and brain. As a result, people with heart failure often feel weak (especially in their arms and legs), tired and have difficulty performing ordinary activities such as walking, climbing stairs or carrying groceries
Nursing Diagnosis
- Activity Intolerance
Related Factors
- Imbalance between oxygen supply/demand
- Generalized weakness
- Prolonged bed rest/immobility
Defining Characteristics
- Weakness, fatigue
- Changes in vital signs, presence of dysrhythmias
- Dyspnea
- Pallor, diaphoresis
Desired Outcomes
- Participate in desired activities; meet own self-care needs.
- Achieve measurable increase in activity tolerance, evidenced by reduced fatigue and weakness and by vital signs within acceptable limits during activity.
Nursing Interventions
For Activity Intolerance nursing diagnosis, nursing interventions include monitoring the patient’s response to activity and gradually performing activity.
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Check vital signs before and immediately after activity, especially if patient is receiving vasodilators, diuretics, or beta-blockers. | Orthostatic hypotension can occur with activity because of medication effect (vasodilation), fluid shifts (diuresis), or compromised cardiac pumping function. |
| Document cardiopulmonary response to activity. Note tachycardia, dysrhythmias, dyspnea, diaphoresis, pallor. | Compromised myocardium and/or inability to increase stroke volume during activity may cause an immediate increase in heart rate and oxygen demands, thereby aggravating weakness and fatigue. |
| Assess for other causes of fatigue (treatments, pain, medications). | Fatigue is a side effect of some medications (beta-blockers, tranquilizers, and sedatives). Pain and stressful regimens also extract energy and produce fatigue. |
| Assess patient’s general condition | To note for any abnormalities and deformities present within the body |
| Therapeutic Interventions | |
| Evaluate accelerating activity intolerance. | May denote increasing cardiac decompensation rather than overactivity. |
| Provide assistance with self-care activities as indicated. Intersperse activity periods with rest periods. | Meets patient’s personal care needs without undue myocardial stress and excessive oxygen demand. |
| Implement graded cardiac rehabilitation program. | Strengthens and improves cardiac function under stress, if cardiac dysfunction is not irreversible. Gradual increase in activity avoids excessive myocardial workload and oxygen consumption. |
| Assist patient with ROM exercises. Check regularly for calf pain and tenderness. | To prevent deep vein thrombosis due to vascular congestion. |
| Adjust client’s daily activities and reduce intensity of level. Discontinue activities that cause undesired psychological changes | Prevents straininga nd overexertion which may aggravate symptoms |
| Instruct client in unfamiliar activities and in alternate ways of conserve energy | Conserves energy and promote safety |
| Encourage patient to have adequate bed rest and sleep | Relaxes the body and promotes comfort |
| Provide the patient with a calm and quiet environment | Provides relaxation |
| Assist the client in ambulation | Prevents risk for falls that could lead to injury |
| Note presence of factors that could contribute to fatigue | Fatigue affects both the client’s actual and perceived ability to participate in activities |
| Ascertain client’s ability to stand and move about and degree of assistance needed or use of equipment | Determines current status and needs associated with participation in needed or desired activities |
| Give client information that provides evidence of daily or weekly progress | Sustains motivation of client |
| Encourage the client to maintain a positive attitude | Enhances sense of well being |
| Assist the client in a semi-fowlers position | Promotes easy breathing |
| Elevate the head of the bed | Maintains an open airway |
| Assist the client in learning and demonstrating appropriate safety measures | Prevents injuries |
| Instruct the SO not to leave the client unattended | Avoids risk for falls |
| Provide client with a positive atmosphere | Helps minimize frustration and rechannel energy |
| Instruct the SO to monitor response of patient to an activity and recognize the signs and symptoms | Indicates need to alter activity level |
Excess Fluid Volume
When blood flow through the renal artery is decreased, the baroreceptor reflex is stimulated and renin is released into the bloodstream. Renin interacts with angiotensinogen to produce angiotensin I. When angiotensin I contacts ACE, it is converted to angiotensin II, a potent vasoconstrictor. Angiotensin II increases arterial vasoconstriction, promote release of norepinephrine from sympathetic nerve endings, and stimulates the adrenal medulla to secrete aldosterone, which enhances sodium and water absorption. Stimulation of the renin-angiotensin system causes plasma volume to expand and preload to increase.
Nursing Diagnosis
- Excess Fluid Volume
Related Factors
- Reduced glomerular filtration rate (decreased cardiac output)/increased antidiuretic hormone (ADH) production, and sodium/water retention.
- Changes in glomerular filtration rate
- Use of diuretics
- Fluid intake or sodium intake
Defining Characteristics
- Orthopnea, S3 heart sound
- Oliguria, edema, JVD, positive hepatojugular reflex
- Weight gain
- Hypertension
- Respiratory distress, abnormal breath sounds
Desired Outcomes
- Demonstrate stabilized fluid volume with balanced intake and output, breath sounds clear/clearing, vital signs within acceptable range, stable weight, and absence of edema.
- Verbalize understanding of individual dietary/fluid restrictions.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Monitor urine output, noting amount and color, as well as time of day when diuresis occurs. | Urine output may be scanty and concentrated (especially during the day) because of reduced renal perfusion. Recumbency favors diuresis; therefore, urine output may be increased at night and/or during bed rest. |
| Monitor and calculate 24-hour intake and output (I&O) balance. | Diuretic therapy may result in sudden increase in fluid loss (circulating hypovolemia), even though edema or ascites remains. |
| Maintain chair or bed rest in semi-Fowler’s position during acute phase. | Recumbency increases glomerular filtration and decreases production of ADH, thereby enhancing diuresis. |
| Establish fluid intake schedule if fluids are medically restricted, incorporating beverage preferences when possible. Give frequent mouth care. Ice chips can be part of fluid allotment. | Involving patient in therapy regimen may enhance sense of control and cooperation with restrictions. |
| Weigh daily. Frequently monitor blood urea nitrogen, creatinine, and serum potassium, sodium, chloride, and magnesium levels. | Documents changes edema in response to therapy. A gain of 5 lb represents approximately 2 L of fluid. Conversely, diuretics can result in excessive fluid shifts and weight loss. |
| Assess for distended neck and peripheral vessels. Inspect dependent body areas for edema (check for pitting); note presence of generalized body edema (anasarca). | Excessive fluid retention may be manifested by venous engorgement and edema formation. Peripheral edema begins in feet and ankles (or dependent areas) and ascends as failure worsens. Pitting edema is generally obvious only after retention of at least 10 lb of fluid. Increased vascular congestion (associated with RHF) eventually results in systemic tissue edema. |
| Auscultate breath sounds, noting decreased and/or adventitious sounds (crackles, wheezes). Note presence of increased dyspnea, tachypnea, orthopnea, paroxysmal nocturnal dyspnea, persistent cough. | Excess fluid volume often leads to pulmonary congestion. Symptoms of pulmonary edema may reflect acute left-sided HF. RHF’s respiratory symptoms (dyspnea, cough, orthopnea) may have slower onset but are more difficult to reverse. |
| Investigate reports of sudden extreme dyspnea and air hunger, need to sit straight up, sensation of suffocation, feelings of panic or impending doom. | May indicate development of complications (pulmonary edema and/or embolus) and differs from orthopnea paroxysmal nocturnal dyspnea in that it develops much more rapidly and requires immediate intervention. |
| Monitor BP and central venous pressure (CVP) | Hypertension and elevated CVP suggest fluid volume excess and may reflect developing pulmonary congestion, HF. |
| Assess bowel sounds. Note complaints of anorexia, nausea, abdominal distension, constipation. | Visceral congestion (occurring in progressive HF) can alter intestinal function. |
| Obtain patient history to ascertain the probable cause of the fluid disturbance. | May include increased fluids or sodium intake, or compromised regulatory mechanisms. |
| Monitor for distended neck veins and ascites | Indicates fluid overload |
| Evaluate urine output in response to diuretic therapy. | Focus is on monitoring the response to the diuretics, rather than the actual amount voided |
| Assess the need for an indwelling urinary catheter. | Treatment focuses on diuresis of excess fluid. |
| Institute/instruct patient regarding fluid restrictions as appropriate. | This helps reduce extracellular volume. |
| Weigh patient daily and compare to previous weights. | Body weight is a sensitive indicator of fluid balance and an increase indicates fluid volume excess. |
| Auscultate breath sounds q 2hr and pm for the presence of crackles and monitor for frothy sputum production | When increased pulmonary capillary hydrostatic pressure exceeds oncotic pressure, fluid moves within the alveolar septum and is evidenced by the auscultation of crackles. Frothy, pink-tinged sputum is an indicator that the client is developing pulmonary edema |
| Assess for presence of peripheral edema. Do not elevate legs if the client is dyspneic. | Decreased systemic blood pressure to stimulation of aldosterone, which causes increased renal tubular reabsorption of sodium Low-sodium diet helps prevent increased sodium retention, which decreases water retention. Fluid restriction may be used to decrease fluid intake, hence decreasing fluid volume excess. |
| Therapeutic Interventions | |
| Follow low-sodium diet and/or fluid restriction | The client senses thirst because the body senses dehydration. Oral care can alleviate the sensation without an increase in fluid intake. |
| Encourage or provide oral care q2 | Heart failure causes venous congestion, resulting in increased capillary pressure. When hydrostatic pressure exceeds interstitial pressure, fluids leak out of the capillaries and present as edema in the legs, and sacrum. Elevation of legs increases venous return to the heart. |
| Change position frequently. Elevate feet when sitting. Inspect skin surface, keep dry, and provide padding as indicated. | Edema formation, slowed circulation, altered nutritional intake, and prolonged immobility (including bed rest) are cumulative stressors that affect skin integrity and require close supervision/ preventive interventions. |
| Provide small, frequent, easily digestible meals. | Reduced gastric motility can adversely affect digestion and absorption. Small, frequent meals may enhance digestion/ prevent abdominal discomfort. |
| Measure abdominal girth, as indicated. | In progressive RHF, fluid may shift into the peritoneal space, causing increasing abdominal girth (ascites). |
| Encourage verbalization of feelings regarding limitations. | Expression of feelings may decrease anxiety, which is an energy drain that can contribute to feelings of fatigue. |
| Palpate abdomen. Note reports of right upper quadrant pain and tenderness. | Advancing HF leads to venous congestion, resulting in abdominal distension, liver engorgement (hepatomegaly), and pain. This can alter liver function and prolong drug metabolism. |
| Administer medications as indicated: | |
|
Signs of potassium and sodium deficits that may occur because of fluid shifts and diuretic therapy. Increases rate of urine flow and may inhibit reabsorption of sodium/ chloride in the renal tubules. |
|
Promotes diuresis without excessive potassium losses. |
|
Replaces potassium that is lost as a common side effect of diuretic therapy, which can adversely affect cardiac function. |
| Maintain fluid and sodium restrictions as indicated. | Reduces total body water and prevent fluid reaccumulation. |
| Consult with dietitian. | May be necessary to provide diet acceptable to patient that meets caloric needs within sodium restriction. |
| Monitor chest x-ray. | Reveals changes indicative of resolution of pulmonary congestion. |
| Assist with rotating tourniquets and/or phlebotomy, dialysis, or ultrafiltration as indicated. | Although not frequently used, mechanical fluid removal rapidly reduces circulating volume, especially in pulmonary edema refractory to other therapies |
Risk for Impaired Gas Exchange
Nursing Diagnosis
- Risk for Impaired Gas Exchange
Risk Factors
- Alveolar-capillary membrane changes, e.g., fluid collection/shifts into interstitial space/alveoli
Desired Outcomes
- Demonstrate adequate ventilation and oxygenation of tissues by ABGs/oximetry within patient’s normal ranges and free of symptoms of respiratory distress.
- Participate in treatment regimen within level of ability/situation.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Auscultate breath sounds, noting crackles, wheezes. | Reveals presence of pulmonary congestion and collection of secretions, indicating need for further intervention. |
| Instruct patient in effective coughing, deep breathing. | Clears airways and facilitates oxygen delivery. |
| Therapeutic Interventions | |
| Encourage frequent position changes. | Helps prevent atelectasis and pneumonia. |
| Maintain chair or bed rest, with head of bed elevated 20–30 degrees, semi-Fowler’s position. Support arms with pillows. | Reduces oxygen demands and promotes maximal lung inflation. |
| Place patient in Fowler’s position and give supplemental oxygen. | To help patient breath more easily and promote maximum chest expansion. |
| Graph graph serial ABGs, pulse oximetry. | Hypoxemia can be severe during pulmonary edema. Compensatory changes are usually present in chronic HF. Note: In patients with abnormal cardiac index, research suggests pulse oximeter measurements may exceed actual oxygen saturation by up to 7%. |
| Administer supplemental oxygen as indicated. | Increases alveolar oxygen concentration, which may reduce tissue hypoxemia. |
| Administer medications as indicated: | |
|
Reduces alveolar congestion, enhancing gas exchange. |
|
Increases oxygen delivery by dilating small airways, and exerts mild diuretic effect to aid in reducing pulmonary congestion. |
Risk for Impaired Skin Integrity
Nursing Diagnosis
- Risk for Impaired Skin Integrity
Risk factors may include
- Prolonged bedrest
- Edema, decreased tissue perfusion
- Decreased activity level
- Prolonged sitting
- Presence of edema
- Altered circulation
Desired Outcomes
- Maintain skin integrity.
- Demonstrate behaviors/techniques to prevent skin breakdown.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Inspect skin, noting skeletal prominences, presence of edema, areas of altered circulation, or obesity and/or emaciation. | Skin is at risk because of impaired peripheral circulation, physical immobility, and alterations in nutritional status. |
| Check fit of shoes and slippers and change as needed. | Dependent edema may cause shoes to fit poorly, increasing risk of pressure and skin breakdown on feet. |
| Therapeutic Interventions | |
| Provide gentle massage around reddened or blanched areas. | Improves blood flow, minimizing tissue hypoxia. Note: Direct massage of compromised area may cause tissue injury. |
| Encourage frequent position changes, assist with active and passive range of motion (ROM) exercises. | Reduces pressure on tissues, improving circulation and reducing time any one area is deprived of full blood flow. |
| Provide frequent skin care: minimize contact with moisture and excretions. | Excessive dryness or moisture damages skin and hastens breakdown. |
| Avoid intramuscular route for medication. | Interstitial edema and impaired circulation impede drug absorption and predispose to tissue breakdown and development of infection. |
| Provide alternating pressure, egg-crate mattress, sheepskin elbow and heel protectors. | Reduces pressure to skin, may improve circulation. |
Deficient Knowledge
Patient education is important in the management and promoting of understanding of heart failure. When the patient recognizes that the diagnosis of HF can be successfully management with lifestyle changes, adherence to therapeutic regimen, and medication, recurrence of acute HF lessen, unnecessary hospitalization decreases, and quality of life improves.
Nursing Diagnosis
- Deficient Knowledge
Related Factors
- Lack of understanding/misconceptions about interrelatedness of cardiac function/disease/failure
Defining Characteristics
- Questioning
- Statements of concern/misconceptions
- Recurrent, preventable episodes of HF
Desired Outcomes
- Identify relationship of ongoing therapies (treatment program) to reduction of recurrent episodes and prevention of complications.
- List signs/symptoms that require immediate intervention.
- Identify own stress/risk factors and some techniques for handling.
- Initiate necessary lifestyle/behavioral changes.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Therapeutic Interventions | |
| Discuss normal heart function. Include information regarding patient’s variance from normal function. Explain difference between heart attack and HF. | Knowledge of disease process and expectations can facilitate adherence to prescribed treatment regimen. |
| Reinforce treatment rationale. Include SOs in teaching as appropriate, especially for complicated regimens such as dobutamine infusion home therapy when patient does not respond to customary combination therapy or cannot be weaned from dobutamine, or those awaiting heart transplant. | Patient may believe it is acceptable to alter postdischarge regimen when feeling well and symptom-free or when feeling below par, which can increase the risk of exacerbation of symptoms. Understanding of regimen, medications, and restrictions may augment cooperation with control of symptoms.
Home IV therapy requires a significant commitment by caregivers to troubleshoot infusion pump, change dressing for peripherally inserted central catheter (PICC) line, monitor I&O and signs and symptoms of HF. |
| Encourage developing a regular home exercise program, and provide guidelines for sexual activity. | Promotes maintenance of muscle tone and organ function for overall sense of well-being. Changing sexual habits may be difficult (sex in morning when well rested, patient on top, inclusion of other physical expressions of affection) but provides opportunity for continuing satisfying sexual relationship. |
| Discuss importance of being as active as possible without becoming exhausted and of rest between activities. | Excessive physical activity or overexertion can further weaken the heart, exacerbating failure, and necessitates adjustment of exercise program. |
| Discuss importance of sodium limitation. Provide list of sodium content of common foods that are to be avoided and limited. Encourage reading of labels on food and drug packages. | Dietary intake of sodium of more than 3 grams per day can offset effect of diuretic. Most common source of sodium is table salt and obviously salty foods, although canned soups, luncheon meats, and dairy products also may contain high levels of sodium. |
| Refer to dietitian for counseling specific to individual dietary customs. | Identifies dietary needs, especially in presence of nausea vomiting and resulting wasting syndrome (cardiac cachexia). Eating six small meals and using liquid dietary supplements and vitamin supplements can limit inappropriate weight loss. |
| Review medications, purpose, and side effects. Provide both oral and written instructions. | Understanding therapeutic needs and importance of prompt reporting of side effects can prevent occurrence of drug-related complications. Anxiety may block comprehension of input or details, and patient/ SO may refer to written material at later date to refresh memory. |
| Recommend taking diuretic early in morning. | Provides adequate time for drug effect before bedtime to prevent interruption of sleep. |
| Instruct and receive return demonstration of ability to take and record daily pulse and blood pressure and when to notify health care provider: parameters above or below preset rate, changes in rhythm and regularity. | Promotes self-monitoring of drug effect. Early detection of changes allows for timely intervention and may prevent complications, such as digitalis toxicity. |
| Explain and discuss patient’s role in control of risk factors (smoking, unhealthy diet) and precipitating or aggravating factors (high-salt diet, inactivity, overexertion, exposure to extremes in temperature). | Adds to body of knowledge, and permits patient to make informed decisions regarding control of condition and prevention of complications. Smoking potentiates vasoconstriction; sodium intake promotes water retention or edema formation; improper balance between activity and rest and exposure to temperature extremes may result in exhaustion and/or increased myocardial workload and increased risk of respiratory infections. Alcohol can depress cardiac contractility. Limitation of alcohol use to social occasions or maximum of 1 drink per day may be tolerated unless cardiomyopathy is alcohol-induced (requiring complete abstinence). |
| Review signs and symptoms that require immediate medical attention: rapid and significant weight gain, edema, shortness of breath, increased fatigue, cough, hemoptysis, fever. | Self-monitoring increases patient responsibility in health maintenance and aids in prevention of complications, e.g., pulmonary edema, pneumonia. Weight gain of more than 3 lb in a week requires medical adjustment of diuretic therapy. Note: Patient should weigh self daily in morning without clothing, after voiding and before eating. |
| Provide opportunities for patient and SO to ask questions, discuss concerns, and make necessary lifestyle changes. | Chronicity and debilitating nature of HF often exhausts coping abilities and supportive capacity of both patient and SO, leading to depression. |
| Discuss general health risks (such as infection), recommending avoidance of crowds and individuals with respiratory infections, obtaining yearly influenza immunization and one-time pneumonia immunization. | This population is at increased risk for infection because of circulatory compromise. |
| Stress importance of reporting signs and symptoms of digitalis toxicity: development of gastrointestinal (GI) and visual disturbances, changes in pulse rate and rhythm, worsening of heart failure. | Early recognition of developing complications and involvement of healthcare provider may prevent toxicity. |
| Identify community resources and support groups and visiting home health nurse as indicated. Encourage participation in an outpatient cardiac rehabilitation program. | May need additional assistance with self-monitoring, home management, especially when HF is progressive. |
| Discuss importance of advance directives and of communicating plan and wishes to family and primary care providers. | Up to 50% of all deaths from heart failure are sudden, with many occurring at home, possibly without significant worsening of symptoms. If patient chooses to refuse life-support measures, an alternative contact person (rather than 911) needs to be designated, should cardiac arrest occur. |
Acute Pain
In ischemic heart disease, atherosclerosis develops in the coronary arteries, causing them to become narrowed or blocked. When a coronary artery is blocked, blood flow to the area of the heart supplied by that artery is reduced. If the remaining blood flow is inadequate to meet the oxygen demands of the heart, the area may become ischemic and injured and myocardial infarction may result. Neural pain receptors are stimulated by local mechanical stress resulting from abnormal myocardial contraction.
Nursing Diagnosis
- Acute Pain
Assessment
Patient may manifest the following
- Difficulty of breathing
- Chest pain
- Restlessness
Planning & Desired Outcomes
- Patient’s pain will be decreased.
- Patient will demonstrate activities and behaviors that will prevent the recurrence of pain.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess patient pain for intensity using a pain rating scale, for location and for precipitating factors. | To identify intensity, precipitating factors and location to assist in accurate diagnosis. |
| Administer or assist with self-administration of vasodilators, as ordered. | The vasodilator nitroglycerin enhances blood flow to the myocardium. It reduces the amount of blood returning to the heart, decreasing preload which in turn decreases the workload of the heart. |
| Assess the response to medications every 5 minutes | Assessing response determines effectiveness of medication and whether further interventions are required. |
| Provide comfort measures. | To provide non pharmacological pain management. |
| Establish a quiet environment. | A quiet environment reduces the energy demands on the patient. |
| Elevate head of bed. | Elevation improves chest expansion and oxygenation. |
| Monitor vital signs, especially pulse and blood pressure, every 5 minutes until pain subsides. | Tachycardia and elevated blood pressure usually occur with angina and reflect compensatory mechanisms secondary to sympathetic nervous system stimulation. |
| Teach patient relaxation techniques and how to use them to reduce stress. | Anginal pain is often precipitated by emotional stress that can be relieved non-pharmacological measures such as relaxation. |
| Teach the patient how to distinguish between angina pain and signs and symptoms of myocardial infarction. | In some case, the chest pain may be more serious than stable angina. The patient needs to understand the differences in order to seek emergency care in a timely fashion. |
Ineffective Tissue Perfusion
Due to decreased cardiac output, there is decreased preload and stroke volume thus there is decreased blood pumped out from the blood. Decrease in stroke volume decreases perfusion throughout the body.
Nursing Diagnosis
- Ineffective Tissue Perfusion
Assessment
- Pale conjunctiva, nail beds, and buccal mucosa
- Generalized weakness
- Chest pain
- Difficulty of breathing
- Abnormal pulse rate and rhythm
- Bradycardia
- Altered BP readings
- With pitting edema on both forearms and hands
- Bipedal pitting edema
Related Factors
- Decreased cardiac output.
Planning & Desired Outcomes
- Patient will demonstrate behaviors to improve circulation.
- Display vital signs within acceptable limits, dysrhythmias absent/controlled,and no symptoms of failure
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess patient pain for intensity using a pain rating scale, for location and for precipitating factors. | To identify intensity, precipitating factors and location to assist in accurate diagnosis. |
| Administer or assist with self administration of vasodilators, as ordered. | The vasodilator nitroglycerin enhances blood flow to the myocardium. It reduces the amount of blood returning to the heart, decreasing preload which in turn decreases the workload of the heart. |
| Assess the response to medications every 5 minutes. | Assessing response determines effectiveness of medication and whether further interventions are required. |
| Give beta blockers as ordered. | Beta blockers decrease oxygen consumption by the myocardium and are given to prevent subsequent angina episodes. |
| Establish a quiet environment. | A quiet environment reduces the energy demands on the patient. |
| Elevate head of bed. | Elevation improves chest expansion and oxygenation. |
| Monitor vital signs, especially pulse and blood pressure, every 5 minutes until pain subsides. | Tachycardia and elevated blood pressure usually occur with angina and reflect compensatory mechanisms secondary to sympathetic nervous system stimulation. |
| Provide oxygen and monitor oxygen saturation via pulse oximetry, as ordered. | Oxygenation increases the amount of oxygen circulating in the blood and, therefore, increases the amount of available oxygen to the myocardium, decreasing myocardial ischemia and pain. |
| Assess results of cardiac markers—creatinine phosphokinase, CK- MB, total LDH, LDH-1, LDH-2, troponin, and myoglobin ordered by physician. | These enzymes elevate in the presence of myocardial infarction at differing times and assist in ruling out a myocardial infarction as the cause of chest pain. |
| Assess cardiac and circulatory status. | Assessment establishes a baseline and detects changes that may indicate a change in cardiac output or perfusion. |
| Monitor cardiac rhythms on patient monitor and results of 12 lead ECG. | Notes abnormal tracings that would indicate ischemia. |
| Teach patient relaxation techniques and how to use them to reduce stress. | Anginal pain is often precipitated by emotional stress that can be relieved non-pharmacological measures such as relaxation. |
| Teach the patient how to distinguish between angina pain and signs and symptoms of myocardial infarction. | In some case, the chest pain may be more serious than stable angina. The patient needs to understand the differences in order to seek emergency care in a timely fashion. |
| Reposition the patient every 2 hours | To prevent bedsores |
| Instruct patient on eating a small frequent feedings | To prevent heartburn and acid indigestion |
Hyperthermia
- Hyperthermia
Assessment
Patient may manifest the following:
- Pale palpebral
- Conjunctiva and nail beds
- Warm to touch
- Weakness
- Increased in body temperature
- Fluid or electrolyte imbalance
- Diaphoresis
- Hot flushed skin
Diagnosis
- Hyperthermia RT increased metabolic rate secondary to pneumonia
Planning & Desired Outcomes
- Patient’s temperature will be on normal level.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess vital signs, the temperature. | Vital signs provide more accurate indication. |
| Monitor and record all sources of fluid loss such as urine, vomiting and diarrhea. | For potential fluid and electrolyte losses. |
| Performed tepid sponge bath. | To promote heat loss by evaporation and conduction. |
| Maintain bed rest. | To reduce metabolic demands and oxygen consumption. |
| Remove excess clothing and covers. | Decreases warmth and increase evaporative cooling. |
| Increase fluid intake. | To prevent dehydration. |
| Provide adequate nutrition, a high caloric diet. | The meet the metabolic demands. |
| Therapeutic Interventions | |
| Control environmental temperature. | To prevent an increase in body temperature and prevent shivering of the patient. |
| Adjust cooling measures on the basis of physical response. | Shivering, which burns calories and increases metabolic rate in order to produce heat. |
| Provide information regarding normal temperature and control. | This is especially necessary for patients with conditions at risk for hyperthermia. |
| Explain all treatments. | Patients’ S.O. needs to be oriented. |
| Administer antipyretics as ordered. | To decrease body temperature. |
| Control excessive shivering with medications such as Chlorpromazine and Diazepam if necessary. | Shivering increases metabolic rate and body temperature. |
| Provide ample fluids by mouth or intravenously as ordered. | If the patient is dehydrated or diaphoretic, fluid loss contributes to fever. |
| Provide oxygen therapy in extreme cases as ordered. | Hyperthermia increases metabolism. |
Ineffective Breathing Pattern
Ineffective Breathing Pattern occurs when there is presence of spasm and inflammation of the lung tissue and parenchyma , these results in inability of the pt to move air in and out of the lungs as needed to maintain adequate tissue oxygenation and perfusion.
Nursing Diagnosis
- Ineffective Breathing Pattern
Assessment
Patient may manifest the following:
- weakness
- rales on BLF
- productive cough
- frothy sputum
- pursed lip breathing
- tachypnea
Diagnosis
- Ineffective breathing pattern related to fatigue and decreased lung expansion and pulmonary congestion secondary to CHF
Planning & Desired Outcomes
- Patient’s respiratory pattern will be effective without causing fatigue
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Establish rapport | To gain comfort feelings form the patient and significant others, |
| Monitor and record vital signs | To gain baseline data |
| Inspect thorax for symmetry of respiratory movement | Determines adequacy of breathing |
| Observe breathing pattern for SOB, nasal flaring, pursed-lip breathing or prolonged expiratory phase and use of accessory muscles | Identifies increased work of breathing |
| Therapeutic Interventions | |
| Measure tidal volume and vital capacity | Indicates volume of air moving in and out of lungs |
| Assess emotional response | Detects use of hyperventilation as a causative factor |
| Position patient in optimal body alignment in semi- fowler’s position for breathing | |
| Assist patient to use relaxation techniques | Reduces muscle tension, decreases work of breathing |
Ineffective Airway Clearance
Mucus is produced at all times by the membranes lining the air passages. When the membranes are irritated or inflamed, excess mucus is produced and it will retain in tracheobronchial tree. The inflammation and increased in secretions block the airways making it difficult for the person to maintain a patent airway. In order to expel excessive secretions, cough reflex will be stimulated. An increase in RR will also be expected as a compensatory mechanism of the body due to obstructed airways.
Nursing Diagnosis
- Ineffective Airway Clearance
Assessment
Patient may manifest the following:
- Rales
- Productive cough
- Difficulty of breathing
Related Factors
- Retained secretions
Planning & Desired Outcomes
- Patient will be able to establish and maintain airway patency
Impaired Gas Exchange
The exchange in oxygenation and carbon dioxide gases is impeded due to the obstruction caused by the accumulation of bronchial secretions in the alveoli. Oxygen cannot diffuse easily.
Nursing Diagnosis
- Impaired Gas Exchange
Defining Characteristics
- Productive cough
- Rales on auscultation
- Difficulty of breathing
- Pale conjunctiva, nail beds and buccal mucosa
- Fatigue
- Metabolic acidosis
- Circumoral cyanosis
Planning & Desired Outcomes
- Patient will be able to demonstrate improvement in gas exchange as evidenced by normal breath sounds, and skin color, presence of eupnea, heart rate 100 bpm or less, Pa02 mm
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess respiratory rate, use of accessory muscles, signs of air hunger, lung excursion, cyanosis, and significant changes in vital signs. | These are warning signs of increasing respiratory distress that requires immediate attention. |
| Auscultate lung fields for presence of crackles. | Decreased breath sound can be a sign of fluid overload or altered ventilation. Crackles signify alveolar fluid congestion and systolic dysfunctional heart failure. On the other hand, wheezing may indicate asthma or related bronchitis. |
| Monitor oxygen saturation and ABG findings. | A pulse oximetry value of 92% or less, decreased PaO2, and increased PaCO2 are signs of decreasing oxygenation. |
| Observe color of skin, mucous membranes and nail beds, noting presence of peripheral cyanosis. | Cyanosis of nail beds may represent vasoconstriction or the body’s response to fever/ chills. |
| Monitor potassium levels. | A possibility of hypokalemia is evident in patients taking diuretics. |
| Therapeutic Interventions | |
| Position the patient in a High Fowler’s position with head of the bed elevated up to 90°. | Promote maximal inspiration, enhance expectoration of secretions in order to improve ventilation. |
| Keep back dry. | To avoid coughing |
| Promote adequate rest periods | Rest will prevent fatigue and decrease oxygen demands for metabolic demands |
| Keep environment allergen free | To reduce irritant effects on airways |
| Suction secretions PRN | To clear airway when secretions are blocking the airway. |
| Administer oxygen therapy as ordered. | Patients with ADHF, high-flow oxygen is given via non non rebreathing mask, positive airway pressure devices, or endotracheal intubation and mechanical intubation. If improves, oxygen is titrated to maintain pulse oximetry readings greater than 92%. |
| Administer diuretics as ordered. | Diuretics promotes normovolemia by decreasing fluid accumulation and blood volume. Fluid overload reduces lung perfusion leading to hypoxemia. |
| Administer vasodilatiors as ordered. | These medications increase venous dilation and decrease pulmonary congestion, that will enhance gas exchange. |
|
Suppresses the effects of the renin-angiotensin system by decreasing angiotensin II and causing reduced secretion of aldosterone. These medications lower blood pressure and decrease preload and afterload, reducing work of the left ventricle. |
|
These are given for patients with intolerance to ACE inhibitors due to cough secondary to the release of bradykinin. |
|
Used in conjunction with nitrates in patients who cannot tolerate medications suchs as ACE inhibitor/ARB due to renal dysfunction. |
|
Acts as a coronary vasodilators and used in combination with hydralazing. |
| Have an airway emergency equipment available at the bedside. | A likelihood of cardiac arrest for patients with severe decompensated heart failure. |
Fatigue
Heart failure is a physiologic state in which the heart cannot pump enough blood to meet the metabolic demands of the body. Since the patient has inadequate cardiac output, it can lead to hypoxic tissue and slowed removal of metabolic wastes, which in turn cause the patient to tire easily.
Nursing Diagnosis
- Fatigue
Assessment
Patient may manifest:
- Weakness
- Limited range of motion
Planning & Desired Outcomes
- Patient will report improved sense of energy
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Review medication regimen. | Certain medications are known to cause or exacerbate fatigue. |
| Assess vital signs. | To evaluate fluid status and cardiopulmonary response to activity. |
| Determine presence or degree of sleep disturbances. | Fatigue can be a consequence of sleep deprivation. |
| Obtain client descriptions of fatigue. | To assist in evaluating impact on client’s life. |
| Ask client to rate fatigue. | To determine degree of fatigability. |
| Therapeutic Interventions | |
| Note daily energy patterns. | Helpful in determining pattern or timing of activity. |
| Establish realistic activity goals with client and encourage forward movement. | Enhances commitment to promoting optimal outcomes. |
| Plan interventions to allow individually adequate rest periods. | To maximize participation. |
| Assist with self-care needs and ambulation. | To conserve energy for other tasks. |
| Avoid exposure to temperature and humidity extremes | Has negative impact on energy level. |
| Instruct client in ways to monitor responses to activity and significant signs or symptoms. | Indicate the need to alter activity level |
| Promote overall health measures | To promote energy |
| Provide supplemental oxygen, as indicated. | Presence of hypoxemia reduces oxygen available for cellular uptakes and contributes to fatigue. |
| Assist client to identify appropriate coping behaviors. | Promote sense of control and improves self-esteem. |
Risk for Decreased Cardiac Tissue Perfusion
Alteration of tissue perfusion is related with dilation, constriction, and occlusion of the blood vessels of the heart.
Nursing Diagnosis
- Ineffective Tissue Perfusion
Risk factors may include
- Atherosclerosis
- Pulmonary congestion
- Presence of edema
Desired Outcomes
- Maintained adequate tissue perfusion as evidenced by blood pressure, pulse rate and rhythm, respiratory rate, and capillary refill within normal limits.
- Demonstrate improvement in mental status.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess changes in mental status such as anxiety, memory loss, confusion, depression, restlessness, lethargy, stupor, and coma. | This may signal reduced cerebral perfusion and decreased oxygen level. |
| Monitor blood pressure every 15 minutes or more frequently if unstable. Watch out for any reduction greater than 20 mm Hg over patient’s baseline or related changes such as dizziness and changes in mental status. | A major side effect of the medical management of heart failure is hypotension which can also be a result of the disease. |
| Monitor heart rate. Monitor for any changes such as tachycardia, arrhythmia. | Indicate decompensation and reduced function of the heart. |
| Assess the extremities for color, temperature, capillary refill, pulse presence and amplitude. | Signs of peripheral vasoconstriction due to sympathetic nervous system compensation includes pallor, coolness, delayed capillary refill time (more than 2 seconds), and decreased pulse amplitude. The presence of edema in the extremities may be observed due to fluid overload |
| Therapeutic Interventions | |
| Administer inotropic, vasodilators as ordered. Watch out for adverse effects that include hypotension, arrhythmia. | |
|
These inotropic drugs enhances the strength of contractions and are kept in case for use in Acute decompensated heart failure (ADHF) related to low-cardiac output and cardiogenic shock until the patient is stabilized. They may be utilized in a long period during advanced-stage HF as a bridge to transplantation or for palliation of symptoms. Use may be associated with increased mortality and ventricular dysrhythmias. Transfer to the coronary care unit may be required for closed monitoring during the administration of these inotropic medications. |
|
These vasodilators are given in Acute decompensated heart failure (ADHF) to reduce cardiac workload by decreasing ventricular filling pressures and systemic vascular resistance. These medications are not recommended for patients with systemic blood pressure less than 90 mm Hg, low-output HF, and cardiogenic shock. |
Fear
Heart failure is a chronic condition that patient may experience a sense of fear with regards of the symptoms, treatment modalities and prognosis of the disease.
Nursing Diagnosis
- Fear
Assessment
- Anticipation of pain
- Anticipation or perceived physical threat or danger
- Threat of death
- Treatment and invasive procedures
Desired Outcomes
- Patient will express fears and concerns and relates obtainment of increasing physical and psychological comfort.
- Patient uses effective coping behaviors to decrease fear.
Nursing Interventions
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Encourage the patient to express fears, feelings regarding the condition. | Recognizing one’s feelings allows communication thus decreases fear. |
| Identify present and past measures that the patient uses to cope with fear. | This information helps determine the effectiveness of coping strategies practiced by the patient. |
| Encourage a calm and quiet environment. | This intervention avoid or decrease the sensory overload that may cause fear. |
| Therapeutic Interventions | |
| Maintain a relaxed and accepting demeanor while communicating with the patient. | The patient’s feeling of stability increases in a peaceful and non-threatening environment. |
| Use simple language and easy to understand statements regarding diagnostic procedures and treatment regimen. | Simple, clear, and brief instructions are important for the patient to understand any given explanations during excessive fear. |
| Provide patient and significant others with emotional support. | Support system from the family and other significant others is important for the patient in decreasing their level of fear. |
| Provide safety measures within the home when indicated (e.g., alarm system, safety devices in showers or bathtubs). | Provide safety measures within the home when indicated (e.g., alarm system, safety devices in showers or bathtubs). |
| Allow the patient to have rest periods. | Relaxation improves ability to cope. The nurse needs to pace activities, especially to older adults to conserve the patient’s energy. |
Anxiety
Anxiety is profoundly frequent among patients with heart failure with nearly 30 percent of patients have clinically significant anxiety symptoms. Anxiety may make it more challenging for patients with heart failure to follow recommendations for diet, exercise, and medication use.
Nursing Diagnosis
- Anxiety
May be related to
- Breathlessness from inadequate oxygenation
Desired Outcomes
- Patient will identify strategies to reduce anxiety.
- Patient will demonstrate improved concentration.
- Patient will manage anxiety and coping patterns.
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess the patient’s level of anxiety. Hildegard E. Peplau described 4 levels of anxiety: mild, moderate, severe and panic. | The patient with mild anxiety will have minimal or no physiological symptoms of anxiety. Vital signs will be within normal ranges. The patient will appear calm but may report feelings of nervousness such as “butterflies in the stomach.”
The patient with moderate anxiety may appear energized, with more animated facial expressions and tone of voice. Vital signs may be normal or slightly elevated. The patient may report feeling tense. With severe anxiety, the patient will have symptoms of increased autonomic nervous system activity, such as elevated vital signs, diaphoresis, urinary urgency and frequency, dry mouth, and muscle tension. At this stage, the patient may experience palpitations and chest pain. The patient may be agitated and irritable and report feeling overloaded or overwhelmed by new stimuli. In the panic level of anxiety, the autonomic nervous system increases to the level of sympathetic neurotransmitter release. The patient becomes pale and hypotensive and experiences poor muscle coordination. The patient reports feeling completely out of control and may display extremes of behavior from combativeness to withdrawal. |
| Assess physical reactions to anxiety. | Anxiety also plays a role in somatoform disorders, which are characterized by physical symptoms such as pain, nausea, weakness, or dizziness that have no apparent physical cause. |
| Validate observations by asking patient, “Are you feeling anxious now?” | Anxiety is a highly individualized, normal physical, and psychological response to internal or external life events. |
| Therapeutic Interventions | |
| Recognize awareness of the patient’s anxiety. | Acknowledgment of the patient’s feelings validates the feelings and communicates acceptance of those feelings. |
| Interact with patient in a peaceful manner. | This approach may help decrease anxiety so that patient’s cardiac work is also decreased. |
| Familiarize patient with the environment and new experiences or people as needed. | Awareness of the environment promotes comfort and may decrease anxiety experienced by the patient. Anxiety may intensify to a panic level if patient feels threatened and unable to control environmental stimuli. A decrease in anxiety will also mean that patient’s cardiac work is also decreased. |
| Administer oxygen during the acute stage. | Oxygen therapy diminishes the work of breathing and to increase comfort. |
| When patient displays anxiety, promote physical comfort and psychological support. | A family member’s presence may provide reassurance; pet visitation or animal-assisted therapy can also be helpful. |
| Converse using a simple language and brief statements. | When experiencing moderate to severe anxiety, patients may be unable to understand anything more than simple, clear, and brief instruction. |
| When patient is comfortable, teach ways to control anxiety and avoid anxiety-provoking situations. | Anxiety may intensify to a panic state with excessive conversation, noise, and equipment around the patient. Increasing anxiety may become frightening to the patient and others. |
| Assist in identifying factors that contribute to anxiety. | Talking about anxiety-producing situations and anxious feelings can help the patient perceive the situation realistically and recognize factors leading to anxious feelings. |
| Help patient determine precipitants of anxiety that may indicate interventions. | Obtaining insight allows the patient to reevaluate the threat or identify new ways to deal with it. |
| Screen fo depression, which often accompanies or results from anxiety. | Symptoms of depression and anxiety are present in about one-third of patients with heart failure. Studies found evidence confirming “markedly higher” rates of depression and anxiety disorders among patients with heart failure, compared to the general population. |
| Allow patient to talk about anxious feelings and examine anxiety-provoking situations if they are identifiable. | Talking about anxiety-producing situations and anxious feelings can help the patient perceive the situation realistically and recognize factors leading to anxious feelings. |
| Assist the patient in developing new anxiety-reducing skills (e.g., relaxation, deep breathing, positive visualization, and reassuring self-statements). | Discovering new coping methods provides the patient with a variety of ways to manage anxiety. |
| Avoid unnecessary reassurance; this may increase undue worry. | Reassurance is not helpful for the anxious individual. |
| Intervene when possible to eliminate sources of anxiety. | Anxiety is a normal response to actual or perceived danger; if the threat is eliminated, the response will stop. |
| Explain all activities, procedures, and issues that involve the patient; use non-medical terms and calm, slow speech. Do this in advance of procedures when possible, and validate patient’s understanding. | With preadmission patient education, patients experience less anxiety and emotional distress and have increased coping skills because they know what to expect. Uncertainty and lack of predictability contribute to anxiety. |
| Educate patient and family about the symptoms of anxiety. | If patient and family can identify anxious responses, they can intervene earlier than otherwise. |
| Teach patient to visualize or fantasize about the absence of anxiety or pain, successful experience of the situation, resolution of conflict, or outcome of procedure. | Use of guided imagery has been useful for reducing anxiety. |
Powerlessness
Patients who are suffering from heart failure may have continuing perception of powerlessness because they are incapable of changing their inevitable outcomes. Powerlessness may be displayed at any time during the patient’s illness and may be observed in the hospital, ambulatory care, rehabilitation, or home environment.
Nursing Diagnosis
- Powerlessness
May be related to
- chronic illness and hospitalizations
Desired Outcomes
- Patient will express sense of personal control.
- Patient displays increased ability to manage self.
- Patient will recognize means to control over personal situation.
| Nursing Interventions | Rationale |
|---|---|
| Nursing Assessment | |
| Assess for factors contributing to a sense of powerlessness. | Identifying the related factors with powerlessness can benefit in recognizing potential causes and building a collaborative plan of care. |
| Assess for feelings of apathy, hopelessness, and depression. | These moods may be an element of powerlessness. |
| Evaluate the patient’s decision-making competence. | Powerlessness is the feeling that one has lost the implicit power to control their own interests. |
| Know situations/interactions that may add to the patient’s sense of powerlessness. | It is necessary for healthcare providers to recognize the patient’s right to refuse certain procedures. Some routines are done on patients without their consent fostering a sense of powerlessness. |
| Appraise the impact of powerlessness on the patient’s physical condition (e.g., appearance, oral intake, hygiene, sleep habits). | Individuals may seem as though they are powerless to establish basic aspects of life and self-care activities. |
| Assess the role of illness plays in the patient’s sense of powerlessness. | The dilemma about events, duration, and course of illness, prognosis, and dependence on others for guidance and treatments can contribute to powerlessness. |
| Evaluate the results of the information given on the patient’s feelings and behavior. | A patient facing powerlessness may overlook information. Too much information may overwhelm the patient and add to feelings of powerlessness. A patient simply experiencing a knowledge deficit may be mobilized to act in his or her own best interest after information is presented and options are explored. The act of providing information about heart failure may strengthen a patient’s sense of independence. |
| Therapeutic Interventions | |
| Listen actively to patient often. | This approach creates a supportive environment and sends a message of caring. |
| Encourage patient to identify strengths. | This will aid patient to recognize inner strengths. |
| Provide patient with decision-making opportunities with increasing frequency and significance. | This approach enhances patient’s independence. |
| Help the patient in reexamining negative perceptions of the situation. | The patient may have his or her own perceptions that are unrealistic for the situation. |
| Provide encouragement and praise while identifying patient’s progress. | This approach creates a supportive environment and sends a message of caring. |
| Assist patient to differentiate between factors that can be controlled and those that cannot. | The patient may have his or her own perceptions that are unrealistic for the situation. |
| Avoid using coercive power when approaching the patient. | This approach may increase the patient’s feelings of powerlessness and result in decreased self-esteem. |
| Eliminate the unpredictability of events by allowing adequate preparation for tests or procedures. | Information in advance of a procedure can provide the patient with a sense of control. |
| Support in planning and creating a timetable to manage increased responsibility in the future. | Use of realistic short-term goals for resuming aspects of self-care foster confidence in one’s abilities. |
Other Heart Failure Nursing Care Plans
Additional nursing diagnosis for heart failure:
- Therapeutic Regimen: ineffective management—complexity of regimen, economic limitations.
- Impaired Home Maintenance — chronic/debilitating condition, insufficient finances, inadequate support systems.
- Self-Care Deficit — decreased strength/endurance, depression.
[td_smart_list_end]
References and Sources
Recommended references and sources for heart failure nursing care plan:
- Black, J. M., & Hawks, J. H. (2009). Medical-surgical nursing: Clinical management for positive outcomes (Vol. 1). A. M. Keene (Ed.). Saunders Elsevier. [Link]
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2016). Nurse’s pocket guide: Diagnoses, prioritized interventions, and rationales. FA Davis. [Link]
- Gulanick, M., & Myers, J. L. (2016). Nursing Care Plans: Diagnoses, Interventions, and Outcomes. Elsevier Health Sciences. [Link]
- Jaarsma, T., Strömberg, A., De Geest, S., Fridlund, B., Heikkila, J., Mårtensson, J., … & Thompson, D. R. (2006). Heart failure management programmes in Europe. European Journal of Cardiovascular Nursing, 5(3), 197-205. [Link]
- Scott, L. D., Setter-Kline, K., & Britton, A. S. (2004). The effects of nursing interventions to enhance mental health and quality of life among individuals with heart failure. Applied Nursing Research, 17(4), 248-256. [Link]
See Also
You may also like the following posts and care plans:
- Nursing Care Plan: The Ultimate Guide and Database – the ultimate database of nursing care plans for different diseases and conditions! Get the complete list!
- Nursing Diagnosis: The Complete Guide and List – archive of different nursing diagnoses with their definition, related factors, goals and nursing interventions with rationale.
Cardiac Care Plans
Nursing care plans about the different diseases of the cardiovascular system:
- Angina Pectoris (Coronary Artery Disease) | 4 Care Plans
- Cardiac Arrhythmia (Digitalis Toxicity) | 3 Care Plans
- Cardiac Catheterization | 4 Care Plans
- Cardiogenic Shock | 5 Care Plans
- Congenital Heart Disease | 5 Care Plans
- Heart Failure | 16+ Care Plans
- Hypertension | 6 Care Plans
- Hypovolemic Shock | 4 Care Plans
- Myocardial Infarction | 7 Care Plans
- Pacemaker Therapy | 7 Care Plans
Originally published on July 14, 2013.
Cholera
This study guide will enable you to learn more about cholera, its risk factors, clinical manifestation, treatment, nursing diagnosis, nursing interventions, and nursing management.
Cholera which continues to be a threat to public health, usually affects individuals who has travel to or live in places with poor sanitation and lack of safe drinking water. This disease is also closely related with poverty, overpopulation, lack of safe disposal of excreta, and unhygienic practices during food preparation, handling and storage.
What is Cholera?
Cholera is an acute diarrhoeal disease caused by Vibrio cholerae.
- Records from Hippocrates (460-377 BCE) and the Indian peninsula describe an illness that might have been cholera.
- Although not the first description, the discovery of the cholera organism is credited to German bacteriologist Robert Koch, who independently identified V cholerae in 1883 during an outbreak in Egypt; the genus name refers to the fact that the organism appears to vibrate when moving.
- The hallmark of the disease is profuse secretory diarrhea.
- Cholera can be endemic, epidemic, or pandemic.
Pathophysiology
Cholera, caused by the bacteria Vibrio cholerae, is a comma-shaped, gram-negative aerobic or facultatively anaerobic bacillus that varies in size from 1-3 µm in length by 0.5-0.8 µm in diameter.
- Currently, the El Tor biotype of V cholerae O1 is the predominant cholera pathogen; organisms in both the classical and the El Tor biotypes are subdivided into serotypes according to the structure of the O antigen.
- The clinical and epidemiologic features of disease caused by V cholerae O139 are indistinguishable from those of disease caused by O1 strains; both serogroups cause clinical disease by producing an enterotoxin that promotes the secretion of fluid and electrolytes into the lumen of the small intestine.
- To reach the small intestine, however, the organism has to negotiate the normal defense mechanisms of the GI tract; because the organism is not acid-resistant, it depends on its large inoculum size to withstand gastric acidity.
- The use of antacids, histamine receptor blockers, and proton pump inhibitors increases the risk of cholera infection and predisposes patients to more severe disease as a result of reduced gastric acidity.
- Fluid loss originates in the duodenum and upper jejunum; the ileum is less affected.
- The colon is usually in a state of absorption because it is relatively insensitive to the toxin; however, the large volume of fluid produced in the upper intestine overwhelms the absorptive capacity of the lower bowel, resulting in severe diarrhea.
- Unless the lost fluid and electrolytes are replaced adequately, the infected person may develop shock from profound dehydration and acidosis from loss of bicarbonate.
- The enterotoxin acts locally and does not invade the intestinal wall. As a result, few neutrophils are found in the stool.
Causes
Cholera can be an endemic, epidemic, or a pandemic disease.
- Environmental factors. Primary infection in humans is incidentally acquired. Risk of primary infection is facilitated by seasonal increases in the number of organisms, possibly associated with changes in water temperature and algal blooms; secondary transmission occurs through fecal-oral spread of the organism through person-to-person contact or through contaminated water and food.
- Host factors. Malnutrition increases susceptibility to cholera. Because gastric acid can quickly render an inoculum of V cholerae noninfectious before it reaches the site of colonization in the small bowel, hydrochlorhydria or achlorhydria of any cause (including Helicobacter pylori infection, gastric surgery, vagotomy, use of H2 blockers for ulcer disease) increases susceptibility; infection rates of household contacts of cholera patients range from 20-50%. Rates are lower in areas where infection is endemic and individuals, especially adults, may have preexisting vibriocidal antibodies from previous encounters with the organism.
Statistics and Incidences
In the United States, cholera has virtually been eliminated because of improved hygiene and sanitation systems.
- The frequency of cholera among international travelers returning to the United States has averaged 1 case per 500,000 population, with a range of 0.05-3.7 cases per 100,000 population, depending on the countries visited.
- Between January 1, 1995, and December 31, 2000, 61 cases of cholera were reported in 18 states and 2 US territories.
- In 1990, fewer than 30,000 cases were reported to the WHO.
- From 2005 to 2008, 178,000-237,000 cases and 4000-6300 deaths were reported annually worldwide.
- In nonendemic areas, the incidence of infection is similar in all age groups, although adults are less likely to become symptomatic than children.
Clinical Manifestations
After a 24- to 48-hour incubation period, symptoms begin with the sudden onset of painless watery diarrhea that may quickly become voluminous and is often followed by vomiting.
- Diarrhea. Profuse watery diarrhea is a hallmark of cholera; cholera should be suspected when a patient older than 5 years develops severe dehydration from acute, severe, watery diarrhea (usually without vomiting) or in any patient older than 2 years who has acute watery diarrhea and is in an area where an outbreak of cholera has occurred.
- Vomiting. Vomiting, although a prominent manifestation, may not always be present; early in the course of the disease, vomiting is caused by decreased gastric and intestinal motility; later in the course of the disease it is more likely to result from acidemia.
- Dehydration. If untreated, the diarrhea and vomiting lead to isotonic dehydration, which can lead to acute tubular necrosis and renal failure; because the dehydration is isotonic, water loss is proportional between 3 body compartments, intracellular, intravascular, and interstitial.
Assessment and Diagnostic Findings
Definitive diagnosis is not a prerequisite for the treatment of patients with cholera.
- Stool examination. Although observed as a gram-negative organism, the characteristic motility of Vibrio species cannot be identified on a Gram stain, but it is easily seen on direct dark-field examination of the stool.
- Stool culture. V cholerae is not fastidious in nutritional requirements for growth; however, it does need an adequate buffering system if fermentable carbohydrate is present because viability is severely compromised if the pH is less than 6, often resulting in autosterilization of the culture.
- Serotyping and biotyping. Specific antisera can be used in immobilization tests; a positive immobilization test result (ie, cessation of motility of the organism) is produced only if the antiserum is specific for the Vibrio type present; the second antiserum serves as a negative control.
- Hematologic tests. Hematocrit, serum-specific gravity, and serum protein are elevated in dehydrated patients because of resulting hemoconcentration; when patients are first observed, they generally have a leukocytosis without a left shift.
- Metabolic panel. Serum sodium is usually 130-135 mmol/L, reflecting the substantial loss of sodium in the stool; serum potassium usually is normal in the acute phase of the illness, reflecting the exchange of intracellular potassium for extracellular hydrogen ion in an effort to correct the acidosis; hyperglycemia may be present, secondary to systemic release of epinephrine, glucagon, and cortisol due to hypovolemia; patients have elevated blood urea nitrogen and creatinine levels consistent with prerenal azotemia.
Medical Management
Rehydration is the first priority in the treatment of cholera. Rehydration is accomplished in 2 phases: rehydration and maintenance.
- Rehydration phase. The goal of the rehydration phase is to restore normal hydration status, which should take no more than 4 hours; set the rate of intravenous infusion in severely dehydrated patients at 50-100 mL/kg/hr; Lactated Ringer solution is preferred over isotonic sodium chloride solution because saline does not correct metabolic acidosis.
- Maintenance phase. The goal of the maintenance phase is to maintain normal hydration status by replacing ongoing losses; the oral route is preferred, and the use of oral rehydration solution (ORS) at a rate of 500-1000 mL/hr is recommended.
- Cholera cots. In areas where cholera is endemic, cholera cots have been used to assess the volume of ongoing stool losses; a cholera cot is a cot covered by a plastic sheet with a hole in the center to allow the stool to collect in a calibrated bucket underneath.
- Diet. Resume feeding with a normal diet when vomiting has stopped; continue breastfeeding infants and young children.
Pharmacological Management
Antimicrobial therapy for cholera is an adjunct to fluid therapy and is not an essential therapeutic component.
- Antibiotics. Empiric antimicrobial therapy must be comprehensive and should cover all likely pathogens in the context of the clinical setting; although not necessarily curative, treatment with an antibiotic to which the organism is susceptible diminishes the duration and volume of the fluid loss and hastens clearance of the organism from stool.
- Vaccines. In June, 2016, the first U.S. cholera vaccine was approved by the FDA; contains live attenuated cholera bacteria that replicate in the gastrointestinal tract of the recipient to provide immunity; it is indicated for active immunization against disease caused by Vibrio cholerae serogroup O1 in adults aged 18-64 y traveling to cholera-affected areas.
Nursing Management
The nursing care of a client with cholera include the following:
Nursing Assessment
Assessment of the patient with cholera are as follows:
- Assess for dehydration. Assess the status of dehydration ( skin color, temperature, skin turgor, mucous membranes, eyes, crown, body temperature, pulse, respiration, behavior, weight loss).
- Observe for diarrhea. Observe for a sudden attack of diarrhea, fever, anorexia, vomiting, nausea, abdominal cramps, increased bowel sounds, and bowel movements more than 3 times a day, with liquid stool consistency, with or without mucus or blood.
- Assess the level of knowledge of the family. Assess for the knowledge of diarrhea at home, dietary knowledge, and knowledge about the prevention of recurrent diarrhea.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnosis for cholera are:
- Deficient fluid volume related to excessive fluid loss through the stool or emesis.
- Imbalanced Nutrition: less than body requirements related to loss of fluids through diarrhea, inadequate intake.
- Risk for infection related to microorganisms that penetrate the gastrointestinal tract.
- Impaired Skin Integrity: perianal, related to irritation from diarrhea.
- Anxiety related to separation from parents, unfamiliar environment, a stressful procedure.
Nursing Care Planning and Goals
The major nursing care planning goals for cholera:
- Patient will maintain adequate hydration.
- Patient will consume adequate nutritional requirements.
- Patient will prevent onset of infection.
- Patient will maintain skin integrity.
- Patient will prevent anxiety.
Nursing Interventions
The nursing interventions on a patient diagnosed with cholera are:
- Monitor intake and output. Note number, character, and amount of stools; estimate insensible fluid losses like diaphoresis; measure urine specific gravity and observe for oliguria.
- Weigh daily. Daily weight is an indicator of overall fluid and nutritional status.
- Maintain hydration. Replace ongoing fluid losses until diarrhea stops.
- Administer medications as indicated. Give an oral antibiotic to the patient with severe dehydration as prescribed.
Evaluation
Nursing goals are met as evidenced by:
- Patient was able to maintain adequate hydration.
- Patient was able to consume adequate nutritional requirements.
- Patient was able to prevent onset of infection.
- Patient was able to maintain skin integrity.
- Patient was able to prevent anxiety.
Documentation Guidelines
Documentation in a patient with cholera include the following:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Practice Quiz: Cholera
Nursing practice questions for cholera. For more practice questions, visit our NCLEX practice questions page.
Exam Mode
In Exam Mode: All questions are shown but the results, answers, and rationales (if any) will only be given after you’ve finished the quiz.
Practice Quiz: Cholera
Practice Mode
Practice Mode: This is an interactive version of the Text Mode. All questions are given in a single page and correct answers, rationales or explanations (if any) are immediately shown after you have selected an answer. No time limit for this exam.
Practice Quiz: Cholera
Text Mode
Text Mode: All questions and answers are given on a single page for reading and answering at your own pace. Be sure to grab a pen and paper to write down your answers.
1. A 90-year-old client is confined to the unit for two weeks. He has been receiving antibiotics for more than a week and tells that he is having frequent watery stools. Which action will you take first?
A. Place the client on contact precautions
B. Educate the client about correct hand washing
C. Notify the physician about the loose stools
D. Get stool specimens for culture
1. Answer: A. Place the client on contact precautions.
- Option A: Prioritization. The client may have Clostridium difficile infection based on his age, history of antibiotic therapy, and watery stools. The initial action should be to place him on contact precautions to prevent the spread of C. difficile to other clients.
- Options B, C, and D: The other actions are also necessary and should be taken after placing the client on contact precautions.
2. A client who has frequent watery stool is admitted to the unit due to dehydration. Which nursing action should the charge nurse delegate to an LPN/LVN?
A. Giving the ordered metronidazole (Flagyl) 500 mg PO to the client
B. Reconsidering the client’s medical history for any risk factors for diarrhea
C. Doing ongoing assessments to determine the client’s hydration status
D. Explaining the purpose of ordered stool cultures to the client family
2. Answer: A. Giving the ordered metronidazole (Flagyl) 500 mg PO to the client.
- Option A: Delegation. LPN/LVN scope of practice and education include administration of medications.
- Options B, C, and D: Assessment of hydration status, client and family education, and assessment of client risk factors for diarrhea should be done by the RN.
3. The nurse is caring for a 20 lbs (9 kg) 6 month-old with a 3-day history of diarrhea, occasional vomiting and fever. Peripheral intravenous therapy has been initiated, with 5% dextrose in 0.33% normal saline with 20 mEq of potassium per liter infusing at 35 ml/hr. Which finding should be reported to the healthcare provider immediately?
A. 3 episodes of vomiting in 1 hour
B. Periodic crying and irritability
C. Vigorous sucking on a pacifier
D. No measurable voiding in 4 hours
3. Answer: D. No measurable voiding in 4 hours.
- Option D: The concern is possible hyperkalemia, which could occur with continued potassium administration and a decrease in urinary output since potassium is excreted via the kidneys.
4. A 5-month old infant was brought by his mother to the health center because of diarrhea occurring 4 to 5 times a day. His skin goes back slowly after a skin pinch and his eyes are sunken. Using the IMCI guidelines, you will classify this infant in which category?
A. No signs of dehydration
B. Some dehydration
C. Severe dehydration
D. The data is insufficient
4. Answer: B. Some dehydration.
- Option B: Using the assessment guidelines of IMCI, a child (2 months to 5 years old) with diarrhea is classified as having SOME DEHYDRATION if he shows 2 or more of the following signs: restless or irritable, sunken eyes, the skin goes back slow after a skin pinch.
5. Based on the assessment, you classified a 3-month old infant with the chief complaint of diarrhea in the category of SOME DEHYDRATION. Based on the IMCI management guidelines, which of the following will you do?
A. Bring the infant to the nearest facility where IV fluids can be given
B. Supervise the mother in giving 200 to 400 ml of Oresol in 4 hours
C. Give the infant’s mother instructions on home management
D. Keep the infant in your health center for close observation
5. Answer: B. Supervise the mother in giving 200 to 400 ml. of Oresol in 4 hours.
- Option B: In the IMCI management guidelines, SOME DEHYDRATION is treated with the administration of Oresol within a period of 4 hours. The amount of Oresol is best computed on the basis of the child’s weight (75 ml/kg body weight). If the weight is unknown, the amount of Oresol is based on the child’s age.
References
Sources and references for this cholera study guide:
Middle East Respiratory Syndrome Coronavirus (MERS-CoV)
Review this study guide to know more about the Middle East respiratory syndrome, its causes, symptoms, treatment, prevention, and nursing management.
MERS or Middle East respiratory syndrome is a zoonotic disease (spreads from animals to people) that can cause severe respiratory illness. It was first identified in Saudi Arabia in 2012 and has infected more than 2,000 individuals worldwide.
What is Middle East Respiratory Syndrome (MERS)?
Middle East respiratory syndrome (MERS) is caused by a novel coronavirus (Middle East respiratory syndrome coronavirus, or MERS‐CoV).
- Through first reported in Saudi Arabia, it was later identified that the first known cases of MERS occurred in Jordan in April 2012.
- Most MERS patients developed severe respiratory illness with symptoms of fever, cough, and shortness of breath.
- A large MERS outbreak occurred in the Republic of South Korea linked to a traveler from the Arabian Peninsula in 2015.
- Travel-associated cases have been identified in Algeria, Austria, China, Egypt, France, Germany, Greece, Italy, Malaysia, Netherlands, Philippines, Republic of Korea, Thailand, Tunisia, Turkey, United Kingdom (UK), and United States (US).
- CDC has published guidance for health departments and healthcare infection-control programs for investigating potential cases of MERS and preventing its spread.
Pathophysiology
MERS is considered an international threat to public health.
- Compared with severe acute respiratory syndrome coronavirus (SARS-Cov), MERS-CoV can establish infection in monocyte-derived macrophages (MDMs) and macrophages.
- The virus induces the release of proinflammatory cytokines, leading to severe inflammation and tissue damage, which may manifest clinically as severe pneumonia and respiratory failure. [
- Vascular endothelial cells located in the pulmonary interstitium may also be infected by MERS-CoV, and, because MERS-CoV receptor DPP4 is expressed in different human cells and tissues, dissemination of the infection may occur.
- Interestingly, lymphopenia has been noted in most patients infected with MERS-CoV, as was noted in SARS infections.
- This is due to cytokine-induced immune cell sequestration and release and induction of monocyte chemotactic protein-1 (MCP-1) and interferon-gamma-inducible protein-10 (IP-10), which suppresses the proliferation of human myeloid progenitor cells.
Causes
Coronaviruses are the largest of all RNA viruses, with positive-sense single-stranded RNA genomes of 26-32 kb.
- Betacoronavirus. MERS-CoV is a recently discovered betacoronavirus of lineage C that was first reported in Saudi Arabia in 2012; the exact origin of this novel coronavirus is still unknown; MERS-CoV is closely related to two coronaviruses of the same lineage found in bats, which may indeed be its wild reservoir.
- Dromedary camels. Specific mechanisms for transmission from animals are unclear but appear to involve contact with dromedary camels or their urine, as well as the consumption of their undercooked meat or unpasteurized dairy products.
Statistics and Incidences
About 3 or 4 out of every 10 patients reported with MERS have died.
- In May 2014, CDC confirmed two unlinked imported cases of MERS in the United States—one to Indiana, the other to Florida; both cases were among healthcare providers who lived and worked in Saudi Arabia; both traveled to the U.S. from Saudi Arabia, where scientists believe they were infected.
- Since 2012, 2,374 laboratory-confirmed cases of infection with MERS-CoV have been reported to the World Health Organization (WHO), including at least 823 related deaths.
- Twenty-seven countries have reported MERS cases.
- On the Arabian Peninsula, countries include Bahrain, Iran, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, United Arab Emirates (UAE), and Yemen.
- Other countries reporting travel-associated MERS include Algeria, Austria, China, Egypt, France, Germany, Greece, Italy, Malaysia, Netherlands, Philippines, Republic of Korea, Thailand, Tunisia, Turkey, United Kingdom (UK), and the United States.
- The vast majority of these cases have so far occurred in the Kingdom of Saudi Arabia.
- The largest MERS outbreak outside of Saudi Arabia occurred in 2015 in the Republic of Korea; the outbreak involved 186 confirmed cases and caused 36 deaths.
- The outbreak sparked quarantine of more than 5,000 individuals and the closure of 2,000 schools before ending.
Clinical Manifestations
Physical examination findings associated with MERS-CoV infection are similar to those presenting with any flu-like symptoms, including the following:
- Fever
- Rhinorrhea, mostly clear
- Pulmonary findings, including hypoxemia, rhonchi, and rales (some patients may have a normal auscultation)
- Tachycardia
- Hypotension may occur with severe illness, reflecting systemic inflammatory response syndrome
Assessment and Diagnostic Findings
Most state laboratories are approved to test for Middle East Respiratory Syndrome Coronavirus (MERS-CoV) using CDC’s rRT-PCR assay.
- rRT-PCR assay. FDA issued an Emergency Use Authorization (EUA) on June 5, 2013, to authorize use of CDC’s 2012 real-time reverse transcription–PCR assay to test for MERS-CoV in clinical respiratory, serum, and stool specimens.
- Serology. Serologic testing for MERS-CoV is available as a research/surveillance test from the CDC; it is not considered a diagnostic test but may offer valuable epidemiologic data; it must be ordered in consultation and with approval of CDC via the EOC.
- Laboratory studies. Laboratory findings at presentation may include leukopenia, lymphopenia, thrombocytopenia, and elevated lactate dehydrogenase levels; these are most likely with increasing severity of illness.
- Imaging studies. Chest imaging findings are abnormal in more than 80% of MERS cases; ground-glass opacity (GGO) is found in over 60% of chest radiographs, with about 20% incidence of consolidation; some infiltrates may be nodular.
Medical Management
Management of the Middle East respiratory syndrome (MERS) coronavirus (MERS-CoV) infection is supportive; this includes hydration, antipyretic, analgesics, respiratory support, and antibiotics if needed for bacterial superinfection.
- Consultations. Upon suspicion of MERS, the patient should be placed in an airborne infection isolation room (AIIR) with a minimum of 12 air exchanges per hour, and personnel protection equipment (PEP) appropriate for contact and airborne precautions (gown, gloves, goggles, and N-95 respirator mask or powered air purifier respirator [PAPR]) should be used.
- Medical care. Medical care is supportive and depends on the severity of illness.
- Prevention. No MERS-CoV vaccine is commercially available; prevention of infection in areas where MERS-CoV is being actively transmitted requires avoidance of potentially infectious secretions and careful attention to hand and respiratory hygiene.
Pharmacologic Management
No medications have been approved for the treatment of coronavirus infections. Clinical trials are needed to establish any benefit from ribavirin and/or interferon alfa.
Nursing Management
Nursing care for a patient with MERS-CoV include the following:
Nursing Assessment
Assessment of a patient with MERS-CoV include:
- History. A high index of suspicion is necessary to suspect MERS, and a travel and exposure history is essential to the diagnosis; keys to the case definition of MERS is a history of residence or travel in the Arabian Peninsula, in countries where MERS-CoV is known to be circulating in dromedary camels, or where human infections have recently occurred and exposure within the incubation period of 14 days.
- Physical exam. Clinical manifestation is indistinguishable from other common respiratory viruses and may range from no symptoms to rapidly progressive multiorgan failure and death.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnosis for a patient with MERS-CoV include the following:
- Infection related to failure to avoid pathogen secondary to exposure to MERS-CoV.
- Deficient knowledge related to unfamiliarity with disease transmission information.
- Hyperthermia related to increase in metabolic rate.
- Ineffective airway clearance related to excessive production of pulmonary secretions.
- Anxiety related to unknown etiology of the disease.
Nursing Care Planning and Goals
The major nursing care plan goals for a patient with MERS-CoV are:
- Prevent the spread of infection.
- Learn more about the disease and its management.
- Reduce increase in temperature.
- Provide a patent airway.
- Reduce anxiety.
Nursing Interventions
Nursing interventions for the patient with MERS-CoV include the following:
- Monitor vital signs. Monitor the patient’s temperature; the infection usually begins with a high temperature; monitor the respiratory rate of the patient as shortness of breath is another common symptom.
- Educate the patient and folks. Include the patient and folks in creating the teaching plan, beginning with establishing objectives and goals for learning at the beginning of the session; provide clear, thorough, and understandable explanations and demonstrations; and give information with the use of media. Use visual aids like diagrams, pictures, videotapes, audiotapes, and interactive Internet websites, such as Nurseslabs.
- Reduce increase in temperature. Adjust and monitor environmental factors like room temperature and bed linens as indicated; encourage ample fluid intake by mouth; eliminate excess clothing and covers, and give antipyretic medications as prescribed.
- Ensure patent airway. Teach the patient the proper ways of coughing and breathing. (e.g., take a deep breath, hold for 2 seconds, and cough two or three times in succession); position the patient upright if tolerated, and encourage patient to increase fluid intake to 3 liters per day within the limits of cardiac reserve and renal function.
- Reduce anxiety. Use presence, touch (with permission), verbalization, and demeanor to remind patients that they are not alone and to encourage expression or clarification of needs, concerns, unknowns, and questions; accept patient’s defenses; do not dare, argue, or debate; converse using a simple language and brief statements; and allow the patient to talk about anxious feelings and examine anxiety-provoking situations if they are identifiable.
Evaluation
Nursing evaluation of goals for a patient with MERS-COV are met as evidenced by:
- Prevention of the spread of infection.
- Acquired knowledge about the disease and its management.
- Reduction in levels of temperature.
- Patent airway achieved.
- Reduction in anxiety.
Documentation Guidelines
Documentation guidelines for a patient with MERS-CoV include the following:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Practice Quiz: Middle East Respiratory Syndrome (MERS)
Nursing practice questions for Middle East Respiratory Syndrome (MERS). For more practice questions, visit our NCLEX practice questions page.
Exam Mode
In Exam Mode: All questions are shown but the results, answers, and rationales (if any) will only be given after you’ve finished the quiz.
Practice Quiz: Middle East Respiratory Syndrome (MERS)
Congratulations - you have completed Practice Quiz: Middle East Respiratory Syndrome (MERS).
You scored %%SCORE%% out of %%TOTAL%%.
Your performance has been rated as %%RATING%%
Practice Mode
Practice Mode: This is an interactive version of the Text Mode. All questions are given in a single page and correct answers, rationales or explanations (if any) are immediately shown after you have selected an answer. No time limit for this exam.
Practice Quiz: Middle East Respiratory Syndrome (MERS)
Congratulations - you have completed Practice Quiz: Middle East Respiratory Syndrome (MERS).
You scored %%SCORE%% out of %%TOTAL%%.
Your performance has been rated as %%RATING%%
Text Mode
Text Mode: All questions and answers are given on a single page for reading and answering at your own pace. Be sure to grab a pen and paper to write down your answers.
1. In which order will the nurse perform the following actions as she prepares to leave the room of a client with airborne precautions after performing oral suctioning?
1. Take off goggles
2. Take off gown
3. Remove gloves
4. Remove N95 respirator
5. Perform hand hygiene
A. 1, 2, 3, 4, 5
B. 2, 1, 4, 3, 5
C. 3, 4, 1, 2, 5
D. 4, 3, 2, 1, 5
1. Answer: B. 2, 1, 4, 3, 5
- Option B: Prioritization. This order will prevent contact of the contaminated gloves and gown with areas like the hair that cannot be readily cleaned after client contact and stop transmission of microorganisms to the nurse and the client. The correct order for donning and removal of PPE has been standardized by agencies such as the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration.
2. The nurse assessed the client and noted shortness of breath and recent trip to China. The client is strongly suspected of having Middle East Respiratory Syndrome (MERS-CoV). Which of these prescribed actions will the nurse take first?
A. Place the client on airborne and contact precautions
B. Introduce normal saline at 75 mL/hr
C. Give methylprednisolone (SOLU-Medrol) 1 g intravenously (IV)
D. Take blood, urine, sputum cultures
2. Answer: A. Place the client on airborne and contact precautions
- Option A: Prioritization. MERS-CoV is considered deadly so the initial action is to protect other clients and healthcare workers by securing the client in isolation. If an airborne-agent isolation (negative-pressure) room is not yet available, droplet precautions should be initiated until the client can be moved to a negative-pressure room.
- Options B, C, and D: The other actions should also be taken immediately but are not as important as preventing transmission of the disease.
3. The school nurse is asked which action will take to have the most impact on the incidence of infectious diseases in school. The correct response is:
A. Grant written information about infection control to all parents
B. Ensure that students are immunized according to national guidelines
C. Make soap and water easily accessible in the classrooms
D. Educate students on how to cover their mouths when coughing
3. Answer: B. Ensure that students are immunized according to national guidelines.
- Option B: Prioritization. The incidence of once-common infectious diseases like measles, chickenpox, and mumps has been most effectively reduced by immunization of all school-aged children.
- Options A, C, and D: The other options are also important but will not have much impact as immunization.
4. Which of the following is the FIRST priority in preventing infections when providing care for a client?
A. Handwashing
B. Wearing gloves
C. Using a barrier between client’s furniture and nurse’s bag
D. Wearing gowns and goggles
4. Answer: A. Handwashing
- Option A: Handwashing remains the most effective way to avoid spreading infection. However, too often nurses do not practice good handwashing techniques and do not teach families to do so. Nurses need to wash their hands before and after touching the client and before entering the nursing bag.
5. A 10-year-old client contracted Middle East Respiratory Syndrome (MERS-CoV) when traveling abroad with her parents. The nurse knows she must put on personal protective equipment to protect herself while providing care. Based on the mode of MERS-CoV transmission, which personal protective should the nurse wear?
A. Gloves
B. Gown and gloves
C. Gown, gloves, and mask
D. Gown, gloves, mask, and eye goggles or eye shield
5. Answer D. Gown, gloves, mask, and eye goggles or eye shield
- Option D: The transmission of MERS-CoV isn’t fully understood. Therefore, all modes of transmission must be considered possible, including airborne, droplet, and direct contact with the virus. For protection from contracting MERS-CoV, any health care worker providing care for a client with MERS should wear a gown, gloves, mask, and eye goggles or an eye shield.
References
Sources and references for this study guide for MERS-COV:
- de Groot, R. J., Baker, S. C., Baric, R. S., Brown, C. S., Drosten, C., Enjuanes, L., … & Perlman, S. (2013). Commentary: Middle East respiratory syndrome coronavirus (MERS-CoV): announcement of the Coronavirus Study Group. Journal of virology, 87(14), 7790-7792. [Link]
- Kimberlin, D. W. (2018). Red Book: 2018-2021 report of the committee on infectious diseases (No. Ed. 31). American academy of pediatrics.
- Oshinsky, D. M. (2005). Polio: an American story. Oxford University Press. [Link]
- Willis, L. (2019). Professional guide to diseases. Lippincott Williams & Wilkins. [Link]
IV Fluids and Solutions Guide & Cheat Sheet (2020 Update)
Get to know the different types of intravenous solutions or IV fluids in this guide and cheat sheet. Differentiate isotonic, hypertonic, and hypotonic IV solutions and the nursing interventions and management for each.
What are IV Fluids?
Intravenous fluids, also known as intravenous solutions, are supplemental fluids used in intravenous therapy to restore or maintain normal fluid volume and electrolyte balance when the oral route is not possible. IV fluid therapy is an efficient and effective way of supplying fluids directly into the intravascular fluid compartment, in replacing electrolyte losses, and in administering medications and blood products.
Types of IV Fluids
There are different types of IV fluids and different ways on how to classify them.
The most common way to categorize IV fluids is based on their tonicity:
- Isotonic. Isotonic IV solutions that have the same concentration of solutes as blood plasma.
- Hypotonic. Hypotonic solutions have lesser concentration of solutes than plasma.
- Hypertonic. Hypertonic solutions have greater concentration of solutes than plasma.
IV solutions can also be classified based on their purpose:
- Nutrient solutions. May contain dextrose, glucose, and levulose to make up the carbohydrate component – and water. Water is supplied for fluid requirements and carbohydrate for calories and energy. Nutrient solutions are useful in preventing dehydration and ketosis. Examples of nutrient solutions include D5W, D5NSS.
- Electrolyte solutions. Contains varying amounts of cations and anions that are used to replace fluid and electrolytes for clients with continuing losses. Examples of electrolyte solutions include 0.9 NaCl, Ringer’s Solution, and LRS.
- Alkalinizing solutions. Are administered to treat metabolic acidosis. Examples: LRS.
- Acidifying solutions. Are used to counteract metabolic alkalosis. D51/2NS, 0.9 NaCl.
- Volume expanders. Are solutions used to increase the blood volume after a severe blood loss, or loss of plasma. Examples of volume expanders are dextran, human albumin, and plasma.
Crystalloids
Crystalloid IV solutions contain small molecules that flow easily across semipermeable membranes. They are categorized according to their relative tonicity in relation to plasma. There are three types: isotonic, hypotonic, and hypertonic.
Isotonic IV Fluids
Most IV fluids are isotonic, meaning, they have the same concentration of solutes as blood plasma. When infused, isotonic solutions expand both the intracellular fluid and extracellular fluid spaces, equally. Such fluids do not alter the osmolality of the vascular compartment. Technically, electrolyte solutions are considered isotonic if the total electrolyte content is approximately 310 mEq/L. Isotonic IV fluids have a total osmolality close to that of the ECF and do not cause red blood cells to shrink or swell.
0.9% NaCl (Normal Saline Solution, NSS)
Normal saline solution (0.9% NaCl) or NSS, is a crystalloid isotonic IV fluid that contains water, sodium (154 mEq/L), and chloride (154 mEq/L). It has an osmolality of 308 mOsm/L and gives no calories. It is called normal saline solution because the percentage of sodium chloride dissolved in the solution is similar to the usual concentration of sodium and chloride in the intravascular space. Normal saline is the isotonic solution of choice for expanding the extracellular fluid (ECF) volume because it does not enter the intracellular fluid (ICF). It is administered to correct extracellular fluid volume deficit because it remains within the ECF.
Normal saline is the IV fluid used alongside the administration of blood products. It is also used to replace large sodium losses such as in burn injuries and trauma. It should not be used for heart failure, pulmonary edema, and renal impairment, or conditions that cause sodium retention as it may risk fluid volume overload.
Dextrose 5% in Water (D5W)
D5W (dextrose 5% in water) is a crystalloid isotonic IV fluid with a serum osmolality of 252 mOsm/L. D5W is initially an isotonic solution and provides free water when dextrose is metabolized (making it a hypotonic solution), expanding the ECF and the ICF. It is administered to supply water and to correct an increase in serum osmolality. A liter of D5W provides fewer than 200 kcal and contains 50g of glucose. It should not be used for fluid resuscitation because hyperglycemia can result. It should also be avoided to be used in clients at risk for increased intracranial pressure as it can cause cerebral edema.
Lactated Ringer’s 5% Dextrose in Water (D5LRS)
Lactated Ringer’s Solution (also known as Ringer’s Lactate or Hartmann solution) is a crystalloid isotonic IV fluid designed to be the near-physiological solution of balanced electrolytes. It contains 130 mEq/L of sodium, 4 mEq/L of potassium, 3 mEq/L of calcium, and 109 mEq/L of chloride. It also contains bicarbonate precursors to prevent acidosis. It does not provide calories or magnesium and has limited potassium replacement. It is the most physiologically adaptable fluid because its electrolyte content is most closely related to the composition of the body’s blood serum and plasma.
Lactated Ringer’s is used to correct dehydration, sodium depletion, and replace GI tract fluid losses. It can also be used in fluid losses due to burns, fistula drainage, and trauma. It is the choice for first-line fluid resuscitation for certain patients. It is often administered to patients with metabolic acidosis.
Lactated Ringer’s solution is metabolized in the liver, which converts the lactate to bicarbonate, therefore, it should not be given to patients who cannot metabolize lactate (e.g., liver disease, lactic acidosis). It should be used in caution for patients with heart failure and renal failure.
Ringer’s Solution
Ringer’s solution is another isotonic IV solution that has content similar to Lactated Ringer’s Solution but does not contain lactate. Indications are the same for Lactated Ringer’s but without the contraindications related to lactate.
Nursing Considerations for Isotonic Solutions
The following are the general nursing interventions and considerations when administering isotonic solutions:
- Document baseline data. Before infusion, assess the patient’s vital signs, edema status, lung sounds, and heart sounds. Continue monitoring during and after the infusion.
- Observe for signs of fluid overload. Look for signs of hypervolemia such as hypertension, bounding pulse, pulmonary crackles, dyspnea, shortness of breath, peripheral edema, jugular venous distention, and extra heart sounds.
- Monitor manifestations of continued hypovolemia. Look for signs that indicate continued hypovolemia such as, decreased urine output, poor skin turgor, tachycardia, weak pulse, and hypotension.
- Prevent hypervolemia. Patients being treated for hypovolemia can quickly develop fluid overload following rapid or over infusion of isotonic IV fluids.
- Elevate the head of the bed at 35 to 45 degrees. Unless contraindicated, position the client in semi-Fowler’s position.
- Elevate the patient’s legs. If edema is present, elevate the legs of the patient to promote venous return.
- Educate patients and families. Teach patients and families to recognize signs and symptoms of fluid volume overload. Instruct patients to notify their nurse if they have trouble breathing or notice any swelling.
- Close monitoring for patients with heart failure. Because isotonic fluids expand the intravascular space, patients with hypertension and heart failure should be carefully monitored for signs of fluid overload.
Hypotonic IV Fluids
Hypotonic IV solutions have a lower osmolality and contain fewer solutes than plasma. They cause fluid shifts from the ECF into the ICF to achieve homeostasis, therefore, causing cells to swell and may even rupture. IV solutions are considered hypotonic if the total electrolyte content is less than 250 mEq/L. Hypotonic IV fluids are usually used to provide free water for excretion of body wastes, treat cellular dehydration, and replace the cellular fluid.
0.45% Sodium Chloride (0.45% NaCl)
Sodium chloride 0.45% (1/2 NS), also known as half-strength normal saline, is a hypotonic IV solution used for replacing water in patients who have hypovolemia with hypernatremia. Excess use may lead to hyponatremia due to the dilution of sodium, especially in patients who are prone to water retention. It has an osmolality of 154 mOsm/L and contains 77 mEq/L sodium and chloride. Hypotonic sodium solutions are used to treat hypernatremia and other hyperosmolar conditions.
0.33% Sodium Chloride (0.33% NaCl)
0.33% Sodium Chloride Solution is used to allow kidneys to retain the needed amounts of water and is typically administered with dextrose to increase tonicity. It should be used in caution for patients with heart failure and renal insufficiency.
0.225% Sodium Chloride (0.225% NaCl)
0.225% Sodium Chloride Solution is often used as a maintenance fluid for pediatric patients as it is the most hypotonic IV fluid available at 77 mOsm/L. Used together with dextrose.
2.5% Dextrose in Water (D2.5W)
Another hypotonic IV solution commonly used is 2.5% dextrose in water (D2.5W). This solution is used to treat dehydration and decreased the levels of sodium and potassium. It should not be administered with blood products as it can cause hemolysis of red blood cells.
Nursing Considerations for Hypotonic Solutions
The following are the general nursing interventions and considerations when administering hypotonic IV solutions:
- Document baseline data. Before infusion, assess the patient’s vital signs, edema status, lung sounds, and heart sounds. Continue monitoring during and after the infusion.
- Do not administer in contraindicated conditions. Hypotonic solutions may exacerbate existing hypovolemia and hypotension causing cardiovascular collapse. Avoid use in patients with liver disease, trauma, or burns.
- Risk for increased intracranial pressure (IICP). Should not be given to patients with risk for IICP as the fluid shift may cause cerebral edema (remember: hypotonic solutions make cells swell).
- Monitor for manifestations of fluid volume deficit. Signs and symptoms include confusion in older adults. Instruct patients to inform the nurse if they feel dizzy.
- Warning on excessive infusion. Excessive infusion of hypotonic IV fluids can lead to intravascular fluid depletion, decreased blood pressure, cellular edema, and cell damage.
- Do not administer along with blood products. Most hypotonic solutions can cause hemolysis of red blood cells especially during rapid infusion of the solution.
Hypertonic IV Fluids
Hypertonic IV solutions have a greater concentration of solutes (375 mEq/L and greater) than plasma and cause fluids to move out of the cells and into the ECF in order to normalize the concentration of particles between two compartments. This effect causes cells to shrink and may disrupt their function. They are also known as volume expanders as they draw water out of the intracellular space, increasing extracellular fluid volume.
Hypertonic Sodium Chloride IV Fluids
Hypertonic sodium chloride solutions contain a higher concentration of sodium and chloride than normally contained in plasma. Infusion of hypertonic sodium chloride solution shifts fluids from the intracellular space into the intravascular and interstitial spaces. Hypertonic sodium chloride IV solutions are available in the following forms and strengths:
- 3% sodium chloride (3% NaCl) containing 513 mEq/L of sodium and chloride with an osmolality of 1030 mOsm/L.
- 5% sodium chloride (5% NaCl) containing 855 mEq/L of sodium and chloride with an osmolality of 1710 mOsm/L.
Hypertonic sodium chloride solutions are used in the acute treatment of sodium deficiency (severe hyponatremia) and should be used only in critical situations to treat hyponatremia. They need to be infused at a very low rate to avoid the risk of overload and pulmonary edema. If administered in large quantities and rapidly, they may cause an extracellular volume excess and precipitate circulatory overload and dehydration. Therefore, they should be administered cautiously and usually only when the serum osmolality has decreased to critically low levels. Some patients may need diuretic therapy to assist in fluid excretion. It is also used in patients with cerebral edema.
Hypertonic Dextrose Solutions
Isotonic solutions that contain 5% dextrose (e.g., D5NSS, D5LRS) are slightly hypertonic since they exceed the total osmolality of the ECF. However, dextrose is quickly metabolized and only the isotonic solution remains. Therefore, any effect on the ICF is temporary. Hypertonic dextrose solutions are used to provide kilocalories for the patient in the short term. Higher concentrations of dextrose (i.e., D50W) are strong hypertonic solutions and must be administered into central veins so that they can be diluted by rapid blood flow.
Dextrose 10% in Water (D10W)
Dextrose 10% in Water (D10W) is an hypertonic IV solution used in the treatment of ketosis of starvation and provides calories (380 kcal/L), free water, and no electrolytes. It should be administered using a central line if possible and should not be infused using the same line as blood products as it can cause RBC hemolysis.
Dextrose 20% in Water (D20W)
Dextrose 20% in Water (D20W) is hypertonic IV solution an osmotic diuretic that causes fluid shifts between various compartments to promote diuresis.
Dextrose 50% in Water (D50W)
Another hypertonic IV solution used commonly is Dextrose 50% in Water (D50W) which is used to treat severe hypoglycemia and is administered rapidly via IV bolus.
Nursing Considerations for Hypertonic Solutions
The following are the general nursing interventions and considerations when administering hypertonic IV solutions:
- Document baseline data. Before infusion, assess the patient’s vital signs, edema status, lung sounds, and heart sounds. Continue monitoring during and after the infusion.
- Watch for signs of hypervolemia. Since hypertonic solutions move fluid from the ICF to the ECF, they increase the extracellular fluid volume and increases the risk for hypervolemia. Look for signs of swelling in arms, legs, face, shortness of breath, high blood pressure, and discomfort in the body (e.g., headache, cramping).
- Monitor and observe the patient during administration. Hypertonic solutions should be administered only in high acuity areas with constant nursing surveillance for potential complications.
- Verify order. Prescription for hypertonic solutions should state the specific hypertonic fluid to be infused, the total volume to be infused, the infusion rate and the length of time to continue the infusion.
- Assess health history. Patients with kidney or heart disease and those who are dehydrated should not receive hypertonic IV fluids. These solutions can affect renal filtration mechanisms and can easily cause hypervolemia to patients with renal or heart problems.
- Prevent fluid overload. Ensure that administration of hypertonic fluids does not precipitate fluid volume excess or overload.
- Do not administer peripherally. Hypertonic solutions can cause irritation and damage to the blood vessel and should be administered through a central vascular access device inserted into a central vein.
- Monitor blood glucose closely. Rapid infusion of hypertonic dextrose solutions can cause hyperglycemia. Use with caution for patients with diabetes mellitus.
Colloids
Colloids contain large molecules that do not pass through semipermeable membranes. Colloids are IV fluids that contain solutes of high molecular weight, technically, they are hypertonic solutions, which when infused, exert an osmotic pull of fluids from interstitial and extracellular spaces. They are useful for expanding the intravascular volume and raising blood pressure. Colloids are indicated for patients in malnourished states and patients who cannot tolerate large infusions of fluid.
Human Albumin
Human albumin is a solution derived from plasma. It has two strengths: 5% albumin and 25% albumin. 5% Albumin is a solution derived from plasma and is a commonly utilized colloid solution. It is used to increase the circulating volume and restore protein levels in conditions such as burns, pancreatitis, and plasma loss through trauma. 25% Albumin is used together with sodium and water restriction to reduce excessive edema. They are considered blood transfusion products and uses the same protocols and nursing precautions when administering albumin.
The use of albumin is contraindicated in patients with the following conditions: severe anemia, heart failure, or known sensitivity to albumin. Additionally, angiotensin-converting enzyme inhibitors should be withheld for at least 24 hours before administering albumin because of the risk of atypical reactions, such as hypotension and flushing.
Dextrans
Dextrans are polysaccharides that act as colloids. They are available in two types: low-molecular-weight dextrans (LMWD) and high-molecular-weight dextrans (HMWD). They are available in either saline or glucose solutions. Dextran interferes with blood crossmatching, so draw the patient’s blood before administering dextran, if crossmatching is anticipated.
Low-molecular-weight Dextrans (LMWD)
LMWD contains polysaccharide molecules that behave like colloids with an average molecular weight of 40,000 (Dextran 40). LMWD is used to improve the microcirculation in patients with poor peripheral circulation. They contain no electrolytes and are used to treat shock related to vascular volume loss (e.g., burns, hemorrhage, trauma, or surgery). On certain surgical procedures, LMWDs are used to prevent venous thromboembolism. They are contraindicated in patients with thrombocytopenia, hypofibrinogenemia, and hypersensitivity to dextran.
High-molecular-weight Dextrans (HMWD)
HMWD contains polysaccharide molecules with an average molecular weight of 70,000 (Dextran 70) or 75,000 (Dextran 75). HMWD used for patients with hypovolemia and hypotension. They are contraindicated in patients with hemorrhagic shock.
Etherified Starch
These solutions are derived from starch and are used to increase intravascular fluid but can interfere with normal coagulation. Examples include EloHAES, HyperHAES, and Voluven.
Gelatin
Gelatins have lower molecular weight than dextrans and therefore remain in the circulation for a shorter period of time.
Plasma Protein Fraction (PPF)
Plasma Protein Fraction is a solution that is also prepared from plasma, and like albumin, is heated before infusion. It is recommended to infuse slowly to increase circulating volume.
Nursing Considerations for Colloid Solutions
The following are the general nursing interventions and considerations when administering colloid IV solutions:
- Assess allergy history. Most colloids can cause allergic reactions, although rare, so take a careful allergy history, asking specifically if they’ve ever had a reaction to an IV infusion before.
- Use a large-bore needle (18-gauge). A larger needle is needed when administering colloid solutions.
- Document baseline data. Before infusion, assess the patient’s vital signs, edema status, lung sounds, and heart sounds. Continue monitoring during and after the infusion.
- Monitor the patient’s response. Monitor intake and output closely for signs of hypervolemia, hypertension, dyspnea, crackles in the lungs, and edema.
- Monitor coagulation indexes. Colloid solutions can interfere with platelet function and increase bleeding times, so monitor the patient’s coagulation indexes.
Cheat Sheet for IV Fluids
In this section is where you can download the cheat sheets for intravenous solutions. Simply click on the images below to open the enlarged image. Please feel free to print, share, and use in your presentations or reports.
References and Sources
The following are the references and sources for this IV fluid guide that you may find interesting or if you want to further your reading:
- Berman, A., Snyder, S. J., Levett-Jones, T., Dwyer, T., Hales, M., Harvey, N., … & Stanley, D. (2018). Kozier and Erb’s Fundamentals of Nursing [4th Australian edition].
- Dougherty, L., & Lamb, J. (Eds.). (2009). Intravenous therapy in nursing practice. John W
- Hinkle, J. L., & Cheever, K. H. (2017). Brunner-Suddarth. Medical-surgical nursing.
Arterial Blood Gas Analysis Made Easy with Tic-Tac-Toe Method
Interpretation of arterial blood gases (ABGs) is a crucial skill that a lot of student nurses and medical practitioners need to learn. In this guide, we’ll help you understand the concepts behind arterial blood gas and teach you the easiest and most fun way to interpret ABGs using the tic-tac-toe method.
What is arterial blood gas?

An arterial blood gas is a laboratory test to monitor the patient’s acid-base balance. It is used to determine the extent of the compensation by the buffer system and includes the measurements of the acidity (pH), levels of oxygen, and carbon dioxide in arterial blood. Unlike other blood samples obtained through a vein, a blood sample from an arterial blood gas (ABG) is taken from an artery (commonly on radial or brachial artery).
What are the components of arterial blood gas?
There are six components of arterial blood gas (ABGs):
pH
The pH is the concentration of hydrogen ions and determines the acidity or alkalinity of body fluids. A pH of 7.35 indicates acidosis and a pH greater than 7.45 indicates alkalosis. The normal ABG level for pH is 7.35 to 7.45.
PaCO2 (Partial Pressure of Carbon Dioxide)
PaCO2 or partial pressure of carbon dioxide shows the adequacy of the gas exchange between the alveoli and the external environment (alveolar ventilation). Carbon dioxide (CO2) cannot escape when there is damage in the alveoli, excess CO2 combines with water to form carbonic acid (H2CO3) causing an acidotic state. When there is hypoventilation in the alveolar level (for example, in COPD), the PaCO2 is elevated, and respiratory acidosis results. On the other hand, when there is alveolar hyperventilation (e.g., hyperventilation), the PaCO2 is decreased causing respiratory alkalosis. For PaCO2, the normal range is 35 to 45 mmHg (respiratory determinant).
PaO2 (Partial Pressure of Oxygen)
PaO2 or partial pressure of oxygen or PAO2 indicates the amount of oxygen available to bind with hemoglobin. The pH plays a role in the combining power of oxygen with hemoglobin: a low pH means there is less oxygen in the hemoglobin. For PaO2, the normal range is 75 to 100 mmHg
SO2 (Oxygen Saturation)
SO2 or oxygen saturation, measured in percentage, is the amount of oxygen in the blood that combines with hemoglobin. It can be measured indirectly by calculating the PAO2 and pH Or measured directly by co-oximetry. Oxygen saturation, the normal range is 94–100%
HCO3 (Bicarbonate)
HCO3 or bicarbonate ion is an alkaline substance that comprises over half of the total buffer base in the blood. A deficit of bicarbonate and other bases indicates metabolic acidosis. Alternatively, when there is an increase in bicarbonates present, then metabolic alkalosis results.
BE (Base Excess)
BE. Base excess or BE value is routinely checked with HCO3 value. A base excess of less than –2 is acidosis and greater than +2 is alkalosis. Base excess, the normal range is –2 to +2 mmol/L
Normal Values in Arterial Blood Gas
To determine acid-base imbalance, you need to know and memorize these values to recognize what deviates from normal. The normal range for ABGs is used as a guide, and the determination of disorders is often based on blood pH. If the blood is basic, the HCO3 level is considered because the kidneys regulate bicarbonate ion levels. If the blood is acidic, the PaCO2 or partial pressure of carbon dioxide in arterial blood is assessed because the lungs regulate the majority of acid. The normal ABG values are the following:
- For pH, the normal range is 7.35 to 7.45
- For PaCO2, the normal range is 35 to 45 mmHg (respiratory determinant)
- For PaO2, the normal range is 75 to 100 mmHg
- For HCO3, the normal range is 22 to 26 mEq/L (metabolic determinant)
- Oxygen saturation, the normal range is 94–100%
- Base excess, the normal range is –2 to +2 mmol/L
Interpreting Arterial Blood Gas Imbalances
Interpreting arterial blood gases is used to detect respiratory acidosis or alkalosis, or metabolic acidosis or alkalosis during an acute illness. To determine the type of arterial blood gas the key components are checked. The best (and fun) way of interpreting arterial blood gas is by using the tic-tac-toe method below:
Goals of ABG analysis
For the purpose of this guide, we have set three (3) goals that we need to accomplish when interpreting arterial blood gases. The goals are as follows:
- Based on the given ABG values, determine if values interpret ACIDOSIS or ALKALOSIS.
- Second, we need to determine if values define METABOLIC or RESPIRATORY.
- Lastly, we need to determine the compensation if it is: FULLY COMPENSATED, PARTIALLY COMPENSATED, or UNCOMPENSATED.
We need to keep these goals in mind as they’ll come up later in the steps for the ABG interpretation technique.
Steps in ABG analysis using the tic-tac-toe method
There are eight (8) steps simple steps you need to know if you want to interpret arterial blood gases (ABGs) results using the tic-tac-toe technique.
1. Memorize the normal values.
The first step is you need to familiarize yourself with the normal and abnormal ABG values when you review the lab results. They are easy to remember:
- For pH, the normal range is 7.35 to 7.45
- For PaCO2, the normal range is 35 to 45
- For HCO3, the normal range is 22 to 26
The recommended way of memorizing it is by drawing the diagram of normal values above. Write it down together with the arrows indicating ACIDOSIS or ALKALOSIS. Note that PaCO2 is intentionally inverted for the purpose of the Tic-Tac-Toe method.
2. Create your tic-tac-toe grid.
Once you’ve memorized the normal values and the diagram, create a blank your tic-tac-toe grid and label the top row as ACIDOSIS, NORMAL, and ALKALOSIS. Based on their values, we need to determine in which column we’ll place pH, PaCO2, and HCO3 in the grid.
3. Determine if pH is under NORMAL, ACIDOSIS, or ALKALOSIS.
The third step of this technique is to determine the acidity or alkalinity of the blood with the given value of the pH as our determining factor. Remember in step #1 that the normal pH range is from 7.35 to 7.45.
- If the blood pH is between 7.35 to 7.39, the interpretation is NORMAL but SLIGHTLY ACIDOSIS, place it under the NORMAL column.
- If the blood pH is between 7.41 to 7.45, interpretation is NORMAL but SLIGHTLY ALKALOSIS, place it under the NORMAL column.
- Any blood pH below 7.35 (7.34, 7.33, 7.32, and so on…) is ACIDOSIS, place it under the ACIDOSIS column.
- Any blood pH above 7.45 (7.46, 7.47, 7.48, and so on…) is ALKALOSIS, place it under the ALKALOSIS column.
Please use the diagram below to help you visualize whether the normal value is ACIDOSIS or ALKALOSIS.
Once you’ve determined whether the pH is under the ACIDOSIS or ALKALOSIS, plot it on your tic-tac-toe grid under the appropriate column.
4. Determine if PaCO2 is under NORMAL, ACIDOSIS, or ALKALOSIS.
For this step, we need to interpret if the value of PaCO2 is within the NORMAL range, ACIDIC, or BASIC and plot it on the grid under the appropriate column. Remember that the normal range for PaCO2 is from 35 to 45:
- If PaCO2 is below 35, place it under the ALKALOSIS column.
- If PaCO2 is above 45, place it under the ACIDOSIS column.
- If PaCO2 is within its normal range, place it under the NORMAL column.
5. Determine if HCO3 is under NORMAL, ACIDOSIS, or ALKALOSIS.
Next, we need to interpret if the value of HCO3 is within the NORMAL range, ACIDIC, or BASIC and plot it under the appropriate column in the tic-tac-toe grid. Remember that the normal range for HCO3 is from 22 to 26:
- If HCO3 is below 22, place it under the ACIDOSIS column.
- If HCO3 is above 26, place it under the ALKALOSIS column.
- If HCO3 is within its normal range, place it under the NORMAL column.
6. Solve for goal #1: ACIDOSIS or ALKALOSIS.
Now, we will start solving for our goals. Looking at the tic-tac-toe grid, determine whether in what column the pH is placed and interpret the results:
- If pH is under the ACIDOSIS column, it is ACIDOSIS.
- If pH is under the ALKALOSIS column, it is ALKALOSIS.
- If pH is under the NORMAL column, determine whether the value is leaning towards ACIDOSIS or ALKALOSIS and interpret accordingly.
In this step, we can accomplish goal #1 of determining ACIDOSIS or ALKALOSIS.
7. Solve for goal #2: METABOLIC or RESPIRATORY.

Looking back again on the tic-tac-toe grid, determine if pH is under the same column as PaCO2 or HCO3 so we can accomplish our goal #2 of determining if the ABG is RESPIRATORY or METABOLIC. Interpret the results as follows:
- If pH is under the same column as PaCO2, it is RESPIRATORY.
- If pH is under the same column as HCO3, it is METABOLIC.
- If pH is under the NORMAL column, determine whether the value is leaning towards ACIDOSIS or ALKALOSIS and interpret accordingly.
8. Solve for goal #3: COMPENSATION.
Lastly, we need to determine the compensation to accomplish our goal #3. Interpret the results as follows:
- It is FULLY COMPENSATED if pH is normal.
- It is PARTIALLY COMPENSATED if all three (3) values are abnormal.
- It is UNCOMPENSATED if PaCO2 or HCO3 is normal and the other is abnormal.
Application and Examples
Let’s solve for the ABG interpretation with the examples below:
Practice Problem #1:
pH=7.26 | PaCO2=32 | HCO3=18
- Remember the normal values.
- Make your tic-tac-toe grid.
- pH of 7.26 ABNORMAL and under ACIDOSIS, so we place pH under ACIDOSIS.
- PaCO2 of 32 is ABNORMAL and under ALKALOSIS, so we place PaCO2 under ALKALOSIS.
- HCO3 of 18 is ABNORMAL and under ACIDOSIS, so we place HCO3 under ACIDOSIS.
- pH is under ACIDOSIS, therefore solving for goal #1, we have ACIDOSIS.
- pH is on the same column as HCO3, therefore solving for goal #2, we have METABOLIC.
- All three values are ABNORMAL, therefore solving for goal #3, we have a PARTIALLY COMPENSATED ABG.
The answer to Practice Problem #1:
Metabolic Acidosis, Partially Compensated
Practice Problem #2:
pH=7.44 | PaCO2=30 | HCO3=21
- Remember the normal values.
- Make your tic-tac-toe grid.
- pH of 7.44 is NORMAL but slightly leaning towards ALKALOSIS, so we place pH under the NORMAL column with an arrow pointing towards the ALKALOSIS column.
- PaCO2 of 30 is ABNORMAL and ALKALOSIS, so we place PaCO2 under the ALKALOSIS column.
- HCO3 of 21 is ABNORMAL and ACIDOSIS, so we place HCO3 under the ACIDOSIS column.
- pH of 7.44 is NORMAL but leaning towards ALKALOSIS, therefore solving for goal #1, we have ALKALOSIS.
- pH is NORMAL but is leaning towards ALKALOSIS, therefore under the same column as PaCO2. Solving for goal #2, we have RESPIRATORY.
- pH is NORMAL, therefore solving for goal #3, we have a FULLY COMPENSATED ABG.
The answer to Practice Problem #2:
Respiratory Alkalosis, Fully Compensated
Practice Problem #3:
pH=7.1 | PaCO2=40 | HCO3=18
- Remember the normal values.
- Make your tic-tac-toe grid.
- pH of 7.1 is ABNORMAL and ACIDOSIS, therefore, we place pH under the ACIDOSIS column in the tic-tac-toe grid.
- PaCO2 of 40 is NORMAL, therefore, place it under the NORMAL column.
- HCO3 of 18 is ABNORMAL and ACIDOSIS, so we place HCO3 under the ACIDOSIS column.
- pH of 7.1 is ACIDOSIS, therefore, solving for goal #1, we have ACIDOSIS.
- pH is under the same column as HCO3, therefore, solving for goal #2, we have determined that it is METABOLIC.
- pH is ABNORMAL so as HCO3, but PaCO3 is under the NORMAL column. Solving for goal #3, we can interpret it as UNCOMPENSATED.
The answer to Practice Problem #3:
Metabolic Acidosis, Uncompensated
How to draw Arterial Blood Gas?
Arterial blood is usually drawn via the brachial or radial artery.
- Inform that client about the procedure and that there is no food or fluid restriction imposed.
- Note if the client is taking anticoagulant therapy or aspirin as this may affect results.
- Note if the client is receiving oxygen therapy (flow rate, type of administration device), and the client’s current temperature.
- Using a heparinized needle and syringe, collect 1 to 5 mL of arterial blood. Common sites for drawing arterial blood are the radial and brachial artery.
- Put the syringe with arterial blood in an ice-water bag to minimize the metabolic activity of the sample.
- Deliver the blood sample immediately to the laboratory.
- Apply pressure to the puncture site for 5 minutes or longer.
Acid-Base Balance and Imbalances
Acid-base imbalances develop when a person’s normal homeostatic mechanisms are dysfunctional or overwhelmed. One type of acid-base imbalance is acidosis wherein the blood is relatively too acidic (low pH). The body produces two types of acid, therefore, there are two types of acidosis: respiratory acidosis and metabolic acidosis. On the contrary, alkalosis is a condition wherein the blood is relatively too basic (high pH), there are also two types of alkalosis: respiratory alkalosis and metabolic alkalosis.
When acid-base imbalances occur, the body activates its compensatory mechanisms (the lungs and kidneys) to help normalize the blood pH. The kidneys compensate for respiratory acid-base imbalances while the respiratory system compensates for metabolic acid-base imbalances. This does not correct the root cause of the problem, if the underlying condition is not corrected, these systems will fail.
Respiratory Acidosis
Respiratory acidosis occurs when breathing is inadequate (alveolar hypoventilation) and the lungs are unable to excrete enough CO2 causing PaCO2 or respiratory acid builds up. The extra CO2 combines with water to form carbonic acid, causing a state of acidosis — a common occurrence in emphysema. The kidneys activate its compensatory process (albeit slow, often 24 hours or more) by increasing the excretion of metabolic acids through urination, which increases blood bicarbonate.
Types of Respiratory Acidosis
There are two forms of respiratory acidosis: Acute and Chronic.
- Acute respiratory acidosis. This form of respiratory acidosis occurs immediately. Left untreated, symptoms will get progressively worse. It’s a medical emergency and can become life-threatening.
- Chronic respiratory acidosis. This form of respiratory acidosis develops through time. It doesn’t cause symptoms. Instead, the body adapts to the increased acidity. For example, the kidneys produce more bicarbonate to help maintain balance. Chronic respiratory acidosis may not cause symptoms. Developing another illness may cause chronic respiratory acidosis to worsen and become acute respiratory acidosis.
Risk Factors
Respiratory acidosis is typically caused by an underlying disease or condition. This is also called respiratory failure or ventilatory failure.
- Hypoventilation. A decrease in ventilation increases the concentration of carbon dioxide in the blood and decreases the blood’s pH (brain trauma, coma, hypothyroidism: myxedema).
- Chronic Obstructive Pulmonary Disease (COPD). In chronic respiratory acidosis in COPD patients, the body tries to compensate by retaining more bicarbonate to overcome acidosis.
- Respiratory Conditions. The lungs are not able to eliminate enough of the carbon dioxide produced by the body. Excess carbon dioxide causes the pH of the blood and other bodily fluids to decrease, making them too acidic. (pneumothorax, pneumonia, status asthmaticus)
- Drug Intake. Overdose of an opiate or opioid, such as morphine, tramadol, heroin, fentanyl, or magnesium sulfate (MgSO4) can cause respiratory acidosis.
Signs and Symptoms
Signs and symptoms of respiratory acidosis are as follows:
- Altered level of consciousness. Respiratory acidosis may be the result of an altered level of consciousness caused by encephalopathy or cerebral edema.
- Confusion. Acute respiratory acidosis may also cause symptoms involving the brain, including confusion, stupor, drowsiness, and muscle jerks.
- Disorientation. Respiratory acidosis may result in disorientation, headache, or even focal neurologic signs.
- Coma. When the lungs can’t remove all of the carbon dioxide produced by the body through normal metabolism, the blood becomes acidified, leading to increasingly serious symptoms, from sleepiness to coma.
- Tremors. Manifest as shaking or jerking muscle movements.
- Asterixis. An inability to maintain the posture of part of the body.
Management of Respiratory Acidosis
Medical and nursing management of an arterial blood gas of respiratory acidosis includes the following:
- Treat underlying conditions.
- Medications. Bronchodilator medicines and corticosteroids may be used to reverse some types of airway obstruction, like those linked to asthma and COPD.
- Weight loss. In the case of obesity hypoventilation syndrome, significant weight loss may be necessary to reduce abnormal compression of the lungs.
- Provide mechanical ventilation through oxygen supplementation. Additional oxygen may be provided to alleviate the low oxygen level in the blood.
- Manage hyperkalemia through the use of Kayexalate. Acidosis causes potassium to move from cells to extracellular fluid (plasma) in exchange for hydrogen ions, and alkalosis causes the reverse movement of potassium and hydrogen ions. Kayexalate increases fecal potassium excretion through the binding of potassium in the lumen of the gastrointestinal tract.
- Maintain adequate hydration. Provide intravenous fluids and electrolytes as ordered.
Respiratory Alkalosis
Respiratory alkalosis can result from hyperventilation since the lungs excrete too much carbonic acid which increases pH. Since respiratory alkalosis occurs quickly, the kidneys do not have time to compensate. Neurological symptoms such as confusion, paresthesias, and cell membrane excitability occur when the blood pH, CSF, and ICF increases acutely.
Risk Factors
Causes of hyperventilation include:
- Panic. Panic attacks and anxiety are the most common causes of hyperventilation.
- Hyperthermia. Fever may manifest as hyperventilation. The exact mechanism is not known but is thought to be due to carotid body or hypothalamic stimulation by the increased temperature.
- Brainstem damage. Central neurogenic hyperventilation (CNH) is the human body’s response to reduced carbon dioxide levels in the blood. This reduction in carbon dioxide is caused by the contraction of cranial arteries from damage caused by lesions in the brain stem.
- Metabolic acidosis. Hyperventilation occurs most often as a response to hypoxia, metabolic acidosis, increased metabolic demands, pain, or anxiety.
- Diabetic ketoacidosis (DKA). The only known compensatory response to metabolic acidosis in DKA is hyperventilation with consecutive respiratory alkalosis.
- Pregnancy. Progesterone levels are increased during pregnancy. Progesterone causes stimulation of the respiratory center, which can lead to respiratory alkalosis.
- Salicylate toxicity. Salicylate toxicity causes respiratory alkalosis and, by an independent mechanism, metabolic acidosis.
Signs and Symptoms
Hyperventilation is a sign that respiratory alkalosis is most likely to occur. However, low carbon dioxide levels in the blood also have a number of physical effects, including:
- Numbness. Increased neuromuscular irritability in which a person loses feeling in a particular part of their body.
- Tingling sensation. Prickling sensation that is usually felt in the hands, arms, legs, or feet, but can also occur in other parts of the body.
- Palpitations. Palpitations are the perceived abnormality of the heartbeat characterized by awareness of cardiac muscle contractions in the chest.
- Tetany. Tetany or tetanic seizure is a medical sign consisting of the involuntary contraction of muscles.
- Convulsions. A medical condition where body muscles contract and relax rapidly and repeatedly, resulting in uncontrolled actions of the body.
- Signs and symptoms of hypokalemia and hypocalcemia. Persistent respiratory alkalosis can induce secondary hypocalcemia and hypokalemia that may cause cardiac arrhythmias, conduction abnormalities, and various somatic symptoms such as paresthesia, hyperreflexia, convulsive disorders, muscle spasm, muscle twitching, positive Chvostek’s sign, and tetany.
Management of Respiratory Alkalosis
The treatment for respiratory alkalosis depends on the underlying cause. Treating the condition is a matter of rising carbon dioxide levels in the blood. The following strategies and tips are useful for respiratory alkalosis caused by over-breathing due to panic and anxiety.
- Breathe into a paper bag. Breathing through a paper bag fills it with carbon dioxide helping in inhaling exhaled air back into the lungs.
- Treat underlying condition:
- Medications. Administering an opioid pain reliever or anti-anxiety medication to reduce hyperventilation.
- Relaxation techniques. Breathing exercises that help relax and breathe from the diaphragm and abdomen, rather than chest wall.
- Safety. Stay with the patient.
- Lavage. After massive aspirin ingestions, aggressive gut decontamination is advisable, including gastric lavage.
- Correction of hypokalemia and hypocalcemia.
- Oxygenation as indicated. Providing oxygen to help keep a person from hyperventilating.
Metabolic Acidosis
Metabolic acidosis is when there is a decrease in bicarbonates and a buildup of lactic acid occurs. This happens in diarrhea, ketosis, and kidney disorders. It has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids.
Risk Factors
- Diabetic Ketoacidosis (DKA). DKA develops when substances called ketone bodies (which are acidic) build up during uncontrolled diabetes. DKA occurs mostly in Type 1 Diabetes Mellitus (DM).
- Chronic Renal Failure (CRF). This is due to reduced tubular bicarbonate reabsorption and insufficient renal bicarbonate production in relation to the number of acids synthesized by the body and ingested with food.
- Chronic Hypoxia. With chronic hypoxia, metabolic and hypercapnic acidosis develop along with considerable lactate formation and pH falling to below 6.8.
- Obesity. Obesity, especially in conjunction with insulin resistance, can increase metabolic acidosis and thus result in a reduction of urinary citrate excretion.
- Diarrhea. Loss of bicarbonate stores through diarrhea or renal tubular wasting leads to a metabolic acidosis state characterized by increased plasma chloride concentration and decreased plasma bicarbonate concentration.
- Dehydration. Electrolyte disturbances caused by prolonged vomiting or severe dehydration can cause metabolic acidosis.
- Aspirin Toxicity. Aspirin overdose causes the body to not produce ATP, leading to anaerobic metabolism with consequent raised lactate and ketone bodies. Acute aspirin or salicylates overdose or poisoning can cause initial respiratory alkalosis through metabolic acidosis ensues thereafter.
- Methanol Poisoning. Significant methanol ingestion leads to metabolic acidosis, which is manifested by a low serum bicarbonate level. The anion gap is increased secondary to high lactate and ketone levels. This is probably due to formic acid accumulation.
Signs and Symptoms
- Altered level of consciousness
- Confusion
- Disorientation
- Lack of appetite
- Coma
- Jaundice
Management of Metabolic Acidosis
Patients with arterial blood gas indicating metabolic acidosis are managed and treated by:
- Sodium bicarbonate. Indicated in the treatment of metabolic acidosis which may occur in severe renal disease, uncontrolled diabetes, circulatory insufficiency due to shock or severe dehydration, extracorporeal circulation of blood, cardiac arrest, and severe primary lactic acidosis.
- Treat the underlying condition.
- Hydration for diabetic ketoacidosis. The major treatment of this condition is the initial rehydration.
- Dialysis for chronic renal failure. The control of metabolic acidosis in hemodialysis is mainly focused on the supply of bicarbonate during the dialysis sessions.
- Use of diuretics.
- Initiate safety measures.
- Kayexalate. Acidosis causes potassium to move from cells to extracellular fluid (plasma) in exchange for hydrogen ions, and alkalosis causes the reverse movement of potassium and hydrogen ions. Kayexalate increases fecal potassium excretion through the binding of potassium in the lumen of the gastrointestinal tract.
Metabolic Alkalosis
Metabolic alkalosis occurs when bicarbonate ion concentration increases, causing an elevation in blood pH. This can occur in excessive vomiting, dehydration, or endocrine disorders.
Risk Factors
- Vomiting. Vomiting causes metabolic alkalosis by the loss of gastric secretions, which are rich in hydrochloric acid (HCl). Whenever a hydrogen ion is excreted, a bicarbonate ion is gained in the extracellular space.
- Sodium bicarbonate overdose. Administration of sodium bicarbonate in amounts that exceed the capacity of the kidneys to excrete this excess bicarbonate may cause metabolic alkalosis.
- Hypokalemia. Due to a low extracellular potassium concentration, potassium shifts out of the cells. In order to maintain electrical neutrality, hydrogen shifts into the cells, raising blood pH.
- Nasogastric suction. Just like in vomiting, nasogastric (NG) suction also generates metabolic alkalosis by the loss of gastric secretions, which are rich in hydrochloric acid (HCl).
Signs and Symptoms
Metabolic alkalosis may not show any symptoms. People with this type of alkalosis more often complain of the underlying conditions that are causing it. These can include:
- Numbness
- Vomiting
- Diarrhea
- Swelling in the lower legs (peripheral edema)
- Fatigue
- Tingling sensation
- Agitation
- Disorientation
- Seizures
- Coma
Management of Metabolic Alkalosis
- Antiemetic. In the case of vomiting, administer antiemetics, if possible.
- Ammonium chloride. Ammonium chloride is a systemic and urinary acidifying agent that is converted to ammonia and hydrochloric acid through oxidation by the liver. Intravenous (IV) ammonium chloride is a treatment option for severe cases of metabolic alkalosis.
- Acetazolamide (Diamox). Acetazolamide also appears to be safe and effective in patients with metabolic alkalosis following treatment of respiratory acidosis from exacerbations of chronic obstructive pulmonary disease (COPD).
ABG Interpretation Quiz
If you need to practice your new skills acquired here, check out our Arterial Blood Gas Interpretation for NCLEX (40 Questions)
References and Sources
The following sources are used as references for this guide. You may find them interesting for your additional reading:
- Barnette, L., & Kautz, D. D. (2013). Creative ways to teach arterial blood gas interpretation. Dimensions of Critical Care Nursing, 32(2), 84-87.
- Samuel, R. (2018). A Graphical Tool for Arterial Blood Gas Interpretation using Standard Bicarbonate and Base Excess. Indian J Med Biochem, 22(1), 85-89.
- Sood, P., Paul, G., & Puri, S. (2010). Interpretation of arterial blood gas. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine, 14(2), 57.
- Williams, A. J. (1998). Assessing and interpreting arterial blood gases and acid-base balance. Bmj, 317(7167), 1213-1216.
- Verma, A. K., & Roach, P. (2010). The interpretation of arterial blood gases. Aust Prescr, 33(4), 124-129.
Chikungunya Virus
Chikungunya is a self-remitting febrile viral disease that has been associated with frequent outbreaks in tropical countries of Africa, Europe, America, and Southeast Asia.
What is Chikungunya Virus?
Chikungunya virus is an insect-borne viral illness that causes sudden onset fever, arthralgia, and rash. It is transmitted to humans through day-biting mosquitoes that belong to the Aedes genus.
- The term “Chikungunya” often refers to both the virus (CHIKV) and the illness or fever (CHIKF) caused by this virus.
- It was derived from the African dialect Swahili or Makonde and translates as “to be bent over”; in Congo, it is referred to as “buka-buka,” which means “broken-broken.”
- These terms refer to the “stooped-over posture” exhibited by individuals with the disease as a consequence of severe chronic incapacitating arthralgias.
- Humans are the primary host of the chikungunya virus during epidemic periods.
Pathophysiology
The exact pathophysiology of Chikungunya virus remains to be investigated. To date, most of the research in this field has been from the Indian subcontinent and other Asian countries.
- Using a murine model, Lum et al have shown that anti–Chikungunya virus antibodies were elicited early in the course of the illness and were directed against the C-terminus of the viral E2 glycoprotein.
- They showed that both natural and Chikungunya virus infection–induced specific antibodies were essential for controlling Chikungunya virus infections.
- The exact mechanism of entry of the virus into mammalian cells is under investigation.
- Bernard et al evaluated this mechanism and found that Chikungunya virus enters mammalian epithelial cells via a clathrin-independent, Esp-15–dependent, dynamin 2–dependent route and requires an endocytic pathway in combination with other unknown pathways.
- Aedes aegypti was known to be the primary vector for Chikungunya infection in India and other countries during the 2006-2010 epidemics.
- Analysis of a 2016 outbreak in Brazil revealed two novel mutations in the virus (K211T in E1 and V156A in E2); these mutations enhanced viral fitness, as they could infect host cells independent of cholesterol, causing the outbreak to become an epidemic.
- Further research in this field would undoubtedly provide a better understanding of the in vivo interactions between Chikungunya virus and immune cells and shed light on the immunopathogenesis.
Statistics and Incidences
Numerous Chikungunya epidemics have been reported in several countries in Southern and South East Asia.
- The first Asian epidemic was reported in Bangkok, Thailand, in 1958, continued until 1964, and reappeared after a hiatus in the mid-1970s and declined again in 1976.
- The most severe Chikungunya fever outbreak was reported in 2006 on Reunion Island, where one-third of the population was infected, resulting in 237 deaths.
- Around the same time, a historical outbreak on the Indian subcontinent involved 1.42 million people, with high morbidity rates.
- According to figures from 2013-2014 from the Centers for Disease Control and Prevention (CDC), European Center for Disease Prevention and Control (ECDC), and the Pan American Health Organization (PAHO), several imported cases of travel-related Chikungunya fever have been reported in the United States, Caribbean islands, Britain, France, Germany, Sweden, Portugal, Canary Islands, and the archipelagos off the coast of Western Africa.
- Chikungunya virus emerged in America in late 2013 and has continued to spread to neighboring countries.
- As of 2017, about 1.8 million cases had been reported from 44 countries.
- A total of 124 cases of Chikungunya virus disease (116 from US states and 8 from US territories) were reported to ArboNET in 2018.
- As of August 1, 2019, a total of 42 Chikungunya virus disease cases had been reported in the United States and its territories in 2019.
Cause
Chikungunya virus is an alpha virus that belongs to the Togaviridae family.
- It is a single-stranded RNA virus and is approximately 11.8 kb long with a capsid and a phospholipid envelope.
- Chikungunya virus is transmitted to humans through day-biting mosquitoes that belong to the Aedes genus.
- Being an arbovirus, the virus is maintained in the environment between humans or other animals and mosquitoes.
- Humans serve as major reservoirs during epidemics.
- During inter-epidemic quiescence in Africa, the virus is thought to be maintained in an epizootic cycle that involves vertebrates such as monkeys, rodents, and birds.
- In Africa, the virus is maintained in a sylvatic cycle among wild primates, monkeys and, wild Aedes mosquitoes (Aedes furcifer, Aedes taylori, Aedes luteocephalus, Aedes africanus, Aedes neoafricanus).
- In Asia, the virus is maintained in an urban cycle involving A aegypti mosquitoes and humans.
Clinical Manifestation
Symptoms usually begin 3–7 days after being bitten by an infected mosquito.
- Fever. One of the most common symptoms is high-grade fevers (up to 105°F).
- Arthralgia. The arthralgias are usually polyarticular and migratory and frequently involve the small joints of the hands, wrist, and ankle, with lesser involvement of the large joints such as the knee or shoulder with associated arthritis; joint pain is worse in the morning, gradually improving with slow exercise and movement but exacerbated by strenuous exercise.
- Cutaneous manifestations. Individuals with Chikungunya fever frequently present with a flushed appearance involving the face and trunk, followed by a diffuse erythematous maculopapular rash of the trunk and extremities, sometimes involving the palms and soles; the rash gradually fades; may evolve into petechiae, urticaria, xerosis, or hyper melanosis; or resolves with desquamation.
- Neurological manifestations. In the acute phase of the illness (reported during the outbreak in the Indian Ocean in 2005-2006), 23 patients presented with neurological symptoms associated with abnormal CSF tests and positive CSF immunoglobulin M (IgM) or reverse-transcriptase polymerase chain reaction (RT-PCR) for Chikungunya virus.
- Others. Rare presentations include severe rheumatoid arthritis, neuroretinitis, uveitis, hearing loss, myocarditis, and cardiomyopathy.
Assessment and Diagnostic Findings
Diagnostic testing is available through a few commercial laboratories, many state health departments, and the Centers for Disease Control and Prevention.
- Serological testing. Chikungunya virus–specific IgM antibodies usually appear upon cessation of viremia, usually by day 5-7 into the illness, and stay positive for 3-6 months; immunoglobulin G (IgG)–neutralizing antibodies appear after 7-10 days and may persist for several months; these antibodies are detected with an enzyme-linked immunoassay (ELISA) test that is available through the CDC and several state health departments.
- Viral culture. Chikungunya virus may be isolated in culture within the first 3 days of illness during the period of active viremia by inoculation of blood into mice or mosquitoes; culture-based detection is also available through the CDC.
- Molecular diagnostics. RT-PCR has been standardized using both structural and nonstructural domains of the Chikungunya virus genome and is available through the CDC.
Medical Management
There is no specific antiviral therapy or vaccine for chikungunya virus infection. Treatment is focused on relieving the symptoms.
- Relieve joint pain and fever. Treatment is for symptoms and can include rest, fluids, and use of non-steroidal anti-inflammatory drugs (NSAIDs) to relieve acute pain and fever.
- Monitor glucose levels. Poor glycemic control in patients with diabetes who have Chikungunya infection has been reported; it is important to monitor the blood glucose closely in these patients.
- Conservative treatment. Conservative treatment includes management of electrolyte imbalance, prerenal azotemia, and hemodynamic monitoring based on severity of illness.
Nursing Management
Nursing care of a patient with Chikungunya virus include:
Nursing Assessment
Assessment of a patient with Chikungunya include:
- History. Chikungunya fever is an acute febrile illness with an incubation period of 3-7 days; it affects all age groups and both sexes equally, with an attack rate (percentage of individuals who develop illness after infection) of 40%-85%.
- Physical examination. Clinical examination reveals high-grade fevers (up to 105°F), pharyngitis, conjunctival suffusion, conjunctivitis, and photophobia; cervical or generalized lymphadenopathy has also been reported in rare cases.
Nursing Diagnosis
Based on the assessment data, the following are some of the nursing diagnoses for patients with Chikungunya:
- Hyperthermia related to increase in metabolic demand.
- Deficient fluid volume related to dehydration.
- Pain related to joint inflammation.
- Impaired skin integrity related to cutaneous manifestations.
Nursing Care Planning and Goals
The major nursing care planning goals in a patient with Chikungunya virus include:
- Patient will improve the body temperature.
- Patient will restore an adequate amount of fluid volume.
- Patient will experience relief from pain.
- Patient will show an improvement of the integrity of the skin.
Nursing Interventions
The nursing interventions for a patient with Chikungunya virus are:
- Improve the body temperature. Eliminate excess clothing and covers; give antipyretic medications as prescribed; perform tepid sponge bath, and modify cooling measures based on the patient’s physical response.
- Restore adequate amount of fluid volume. Assess skin turgor and oral mucous membranes for signs of dehydration; assess color and amount of urine and report urine output less than 30 ml/hr for 2 consecutive hours; urge the patient to drink the prescribed amount of fluid, and administer parenteral fluids as prescribed.
- Relief from pain. Acknowledge reports of pain immediately; provide rest periods to promote relief, sleep, and relaxation; and provide analgesics as ordered, evaluating the effectiveness and inspecting for any signs and symptoms of adverse effects.
- Improve the integrity of the skin. Monitor site of impaired tissue integrity at least once daily for color changes, redness, swelling, warmth, pain, or other signs of infection; provide tissue care as needed; tell the patient to avoid rubbing and scratching; provide gloves or clip the nails if necessary; administer antibiotics as ordered.
Evaluation
Nursing Goals are met as evidenced by:
- Improve the body temperature.
- Restore adequate amount of fluid volume.
- Relief from pain.
- Improve integrity of the skin.
Documentation Guidelines
Documentation in a patient with Chikungunya virus include the following:
- Individual findings, including factors affecting, interactions, nature of social exchanges, specifics of individual behavior.
- Cultural and religious beliefs, and expectations.
- Plan of care.
- Teaching plan.
- Responses to interventions, teaching, and actions performed.
- Attainment or progress toward the desired outcome.
Summary
Here are some of the most important points about Chikungunya virus:
- Chikungunya fever is a self-remitting febrile viral illness that has been associated with frequent outbreaks in tropical countries of Africa and Southeast Asia.
- Chikungunya virus is transmitted to humans through day-biting mosquitoes that belong to the Aedes genus.
- Numerous Chikungunya epidemics have been reported in several countries in Southern and Southeast Asia.
- Chikungunya virus is an alphavirus that belongs to the Togaviridae family.
- Symptoms usually begin 3–7 days after being bitten by an infected mosquito, and these include fever, arthralgia, cutaneous manifestations, and neurological manifestations.
- There is no specific antiviral therapy for chikungunya virus infection.
Practice Quiz: Chikungunya Virus
Nursing practice questions for Chikungunya virus. For more practice questions, visit our NCLEX practice questions page.
1. The following statements are true regarding the Chikungunya virus, except:
A. Chikungunya is caused by a Flavirideae flavivirus.
B. It is most commonly seen to occur in the tropical regions of Asia, Africa, and South America.
C. Chikungunya has a shorter incubation period than dengue fever.
D. The disease causes polyarthralgia, headache, swelling, and rash.
E. There is no vaccine available for this disease.
1. Answer: A. Chikungunya is caused by a Flavirideae flavivirus.
• Option A: Flaviridaeae flavivirus causes Dengue fever. Chikungunya is caused by a virus of the genus alphavirus and belonging to the family Togaviridae.
2. Which mosquito genus is associated with spreading the Chikungunya virus?
A. Culex
B. Anopheles
C. Aedes
D. Lutzia
2. Answer: C. Aedes.
• Option C: Chikungunya virus is transmitted to humans through day-biting mosquitoes that belong to the Aedes genus.
3. Nurse Layla is conducting a health seminar to a group of adults in a rural area in Myanmar. Which of the following measures will provide the most protection against mosquito-borne diseases, except?
A. Removing old tires, buckets, and potted plant trays
B. Applying 10% DEET-based repellant
C. Wearing long-sleeved shirts and pants
D. Staying in places that have door screen and windows
E. None of the above
3. Answer: B. Applying 10% DEET-based repellant
• Option B: The Center for Disease Control and Prevention (CDC) recommends using a repellant that contains 20% or more diethyltoluamide (DEET), the most active ingredient in insect repellants especially to places with a high risk of mosquito-borne diseases such as in Myanmar.
4. Appropriate nursing diagnoses for clients who are taking NSAIDs would be which of the following?
A. Risk for injury related to prolonged bleeding time, inhibition of platelet aggregation, and increased risk of GI bleeding.
B. Potential for injury related to GI toxicity and a decrease in bleeding time.
C. Altered protection related to GI bleeding and increasing platelet aggregation.
D. Risk for injury related to thrombocytosis prolonged prothrombin time.
4. Answer: A. Risk for injury related to prolonged bleeding time, inhibition of platelet aggregation, and increased risk of GI bleeding.
• Option A: The nursing diagnosis addresses all the interactions that pose a threat to the client taking both these drugs.
• Option B: Bleeding time is prolonged not decreased when both drugs are used.
• Option C: Platelet aggregation is inhibited not increased when both drugs are used.
• Option D: Thrombocytosis does not occur with the use of either drug.
5. Which of the following groups of clients are most at risk for GI bleeding from the use of NSAIDs?
A. Clients with dysmenorrhea
B. Clients with headaches
C. Clients with arthritis
D. Clients with renal failure
5. Answer: C. Clients with arthritis.
• Option C: Clients with arthritis are taking the drug for prolonged periods of time and may take higher doses.
•Options A & B: Choices A and B are incorrect because the use of NSAIDs with these clients is intermittent.
• Option D: Renal failure is a contraindication for NSAIDs because most of the drug is excreted through the kidneys.
References
Sources and references for this Chikungunya study guide:
• Centers for Disease Control and Prevention. (2019, Sept 19). Chikungunya. Retrieved from https://www.cdc.gov/chikungunya/index.html
• Natesan, S.K. (2019, Aug 1). Chikungunya virus. Retrieved from https://emedicine.medscape.com/article/2225687-overview